 Testicular cancer is the most common cancer in males between the ages of 15 and 35. The cancer originates within the testicles, which are responsible for producing sperm for reproduction and also produce male sex hormones like testosterone.
Testicular cancer is the most common cancer in males between the ages of 15 and 35. The cancer originates within the testicles, which are responsible for producing sperm for reproduction and also produce male sex hormones like testosterone.
The cells that eventually form sperm (termed germ cells) are the origin of most testicular cancers. The cancer is relatively rare but is highly treatable. At Comprehensive Urology, a testicular cancer surgeon will guide you patients through all stages of the diagnosis and treatment of the disease. Call (310) 499-2756 or contact us online today for a consultation on your needs!
Signs and Symptoms of Testicular Cancer
Men can have different signs and symptoms that can lead to the diagnosis of testicular cancer. Common testicular cancer symptoms include:
- Pain in the testicle or groin
- Enlargement of the scrotum
- Mass felt in the testicle
- Loss of energy
Risk Factors
There are certain risk factors associated with testicular cancer. Beverly Hills doctors at Comprehensive Urology can help identify these risk factors, which can include the following:
Race
Caucasians have a higher risk than African Americans
Age
Younger men (ages 15-35) have higher risk of developing this disease than older men
Undescended Testicle
The testicles develop in the abdomen before birth and slowly descend into the scrotum before birth. Some children are born with a testicle that has not descended in the scrotum. In adulthood, these men have an increased risk of developing cancer in the testicle even if surgically repaired as a child. The increased risk also applies to the testicle that had descended normally before birth. A testicular cancer specialist can help determine treatment options for an undescended testicle.
History of Testicular Cancer
A man who has been diagnosed with testicular cancer in one testicle has a slightly increased risk of developing cancer in the remaining testicle, although the overall risk is still low. In certain cases, patients may require testicular cancer treatment, such as testicular cancer surgery, in order to fight the disease.
Family History
Men who know family members who were diagnosed with this disease may be at increased risk.
Infertility & Family Planning After Testicular Cancer
Most men who have been diagnosed with testicular cancer are concerned about the possibility of becoming infertile after treatment. There are many different treatments for testicular cancer and the short and long term effects may vary.
Testicular Cancer Treatments and Their Effect on Fertility
 If you are considering testicular cancer treatments and would like to take into account their effects on fertility, the following information can help you stay informed and be prepared.
If you are considering testicular cancer treatments and would like to take into account their effects on fertility, the following information can help you stay informed and be prepared.
Surgery
Typically, removing a testicle does not have a serious effect on a man’s sexual performance or his ability to procreate. This is because once one the cancerous testicle is removed, the remaining, healthy testicle will produce more testosterone and sperm to make up for what was lost. Most men will still be able to have an erection, however, the orgasm may feel different because it will be a dry climax. Although surgical removal of a testicle has no negative impact on a man’s fertility, some still consider storing sperm regardless.
Chemotherapy
Although chemotherapy does not affect a man’s ability to have sex, most men complain of little to no sex drive for a period of time after treatment. Unfortunately, chemotherapy has been shown to cause infertility, so your doctor may strongly advise you to store sperm prior to treatment. The higher the dose of chemotherapy, the higher the risk of causing infertility.
Radiotherapy
Radiotherapy may be given as an alternative or in addition to chemotherapy treatment, especially if the cancer has spread elsewhere in the body. Radiotherapy to the nodes in the abdomen does not affect a man’s ability to have sexual intercourse and does not usually cause infertility. However, just like with surgical procedures, it might be a good idea to store sperm anyway.
Contraception During Treatment
Men with testicular cancer are strongly advised not to pursue conception during chemotherapy or radiotherapy treatment. Mainly, this is because these types of treatment can damage your sperm and possibly harm a baby conceived at this time. Medical professionals usually advise men to avoid conceiving a child for about a year after treatment has ended, which will allow the sperm to recover from any damage that chemotherapy or radiotherapy may have caused. Fortunately, many men who have been treated for testicular cancer are able to have families after they are fully recovered.
Testosterone Replacement Therapy
Generally, having one testicle removed does not usually hinder a man’s sex drive since the healthy testicle will make enough testosterone to compensate for the other. In some cases, however, the remaining testicle does not produce enough testosterone. In even rarer cases, a man may need to have both testicles removed from an advanced case of testicular cancer.
A lack of testosterone may affect a man’s ability to get an erection and may reduce his sex drive. Other symptoms may include tiredness, low energy and osteoporosis, which is a condition characterized by the thinning of bones. If you are experiencing any of these symptoms, your doctor may measure your testosterone levels to see if you are a good candidate for testosterone replacement therapy. This can be given as a gel, an injection into a muscle, an implant or as a patch that is attached to the skin. Men who go through testosterone replacement therapy are usually able to increase their sex drive and regain their energy.
Preserving Fertility After Testicular Cancer Treatment
Although most men are still able to father children after testicular cancer treatment, the fertility of some men after treatment is hampered. This is due to the type and amount of treatment needed to treat the cancer. Going through cancer is difficult enough without the possibility of being unable to conceive a child. Fortunately, there are possible methods to preserving a man’s fertility.
Storing Sperm (Sperm Banking)
Sperm banking is a common and safe technique that has been used for many years. It involves the freezing of your sperm. This is strongly recommended for men who will need to receive chemotherapy, which is damaging to the sperm. However, even if your risk of becoming infertile are low, your doctor may still advise you to store two to three samples of sperm.
The fertility clinic will usually provide counseling before you freeze your sperm. You will also need to sign a consent form that states how your sperm will be used in the future. You will also need to take a blood test to rule out any diseases such as HIV or hepatitis. Once you are fully recovered from treatment and ready to have a child, your sperm can be thawed and used with fertility treatments. Sperm samples can be kept frozen until the age of 55. Not all men are eligible for sperm banking as they need to begin treatment for testicular cancer immediately. It is best to discuss your options with your doctor.
Intra-Cytoplasmic Sperm Injection (ICSI)
ICSI is an option for men who are not producing many sperm or for those who will need to begin cancer treatment quickly. This fertility treatment only needs a single sperm to fertilize an egg.
Extraction of Testicular Tissue or Fluid
A newer fertility technique in sperm by extracting a piece of testicular tissue or fluid. Small amounts of fluid or tissue are removed by inserting a needle into the testicle, or by making a small cut in the scrotum. The fluid or tissue is examined, followed by removing and storage of the sperm for future use.
Testicular Cancer Screening & Diagnosis
 We encourage all men in the higher risk age group (15-35) to regularly perform self-examinations to check for abnormal lumps in their testicles. We also encourage all of our patients to see their doctor for their routine physical examination where masses are also often detected.
We encourage all men in the higher risk age group (15-35) to regularly perform self-examinations to check for abnormal lumps in their testicles. We also encourage all of our patients to see their doctor for their routine physical examination where masses are also often detected.
When a testicular cancer is suspected on physical exam or screening, our physician will routinely order further tests to assist with the diagnosis.
Diagnosis of Testicular Cancer
When a testicular cancer is suspected, our physicians routinely order further tests to assist with the diagnosis. These include:
Testicular Ultrasound
This test involves sound waves that are bounced off internal organs to make echoes and form a picture of the organ being investigated. The picture can help confirm whether a mass is present within the testicle.
Serum Tumor Markers
Your physician will order blood tests to detect substances that are typically released by some types of testicular cancer and can therefore be found in increased concentrations in the blood. These blood tests can also be used to follow the patient’s response to treatments after the diagnosis has been made, and can help guide treatments as well. These tumor markers include Alpha-Fetoprotein (AFP) and Beta Human Chorionic Gonadotropin (β-HCG).
Radical Orchiectomy
After the above tests have been performed, the definitive diagnosis of testicular cancer is made by an outpatient procedure termed Radical Orchiectomy. A small incision is made in the lower groin in order to evaluate and remove the testicle suspected of harboring the cancer. If cancer is found, it is further evaluated to determine the exact cell type(s) to help guide treatment
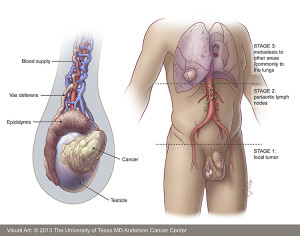
Once testicular cancer has been diagnosed, your doctor will order a number of tests to help determine the stage of the disease (to see if the cancer has spread to other areas).
Staging of Testicular Cancer
Once Testicular Cancer has been diagnosed, your doctor will order a number of tests to help determine the stage of the disease (to see if the cancer has spread to other areas).
CT Scan
This is a study which takes a number of detailed images of the chest, abdomen and pelvis to see if the lymph nodes appear abnormal, indicating possible spread of testicular cancer into these areas.
Repeat Tumor Markers
If these markers (AFP and β-HCG) are elevated prior to orchiectomy, your physician will follow these markers after orchiectomy to ensure they have normalized in the blood appropriately. If they do not normalize within a certain period after orchiectomy, this may indicate persistent cancer within the body.
After these tests are performed, your physician will be able to stage the disease.
Stage 1: Cancer only within the testis
Stage 2: Cancer found within the abdominal lymph nodes
Stage 3: Cancer has spread elsewhere within the body (for example, the chest, bones, brain)
Orchiectomy
 Many men experience decreased sperm counts with testicular cancer itself, which often improves after treatment. Some cancer treatments can also cause infertility as well. Radical Orchiectomy (removal of the testicle that contains the tumor) will not cause infertility. It may actually help restore normal sperm production if the tumor is confined only to the testicle itself. After the diagnosis of testicular cancer with radical orchiectomy, we encourage our patients to perform sperm banking prior to any additional therapy to help cure the disease even if they are not planning to have any more children in the future. Chemotherapy and radiation can lead to temporary infertility for 1-2 years, but in a smaller percentage of patients, the infertility can be permanent.
Many men experience decreased sperm counts with testicular cancer itself, which often improves after treatment. Some cancer treatments can also cause infertility as well. Radical Orchiectomy (removal of the testicle that contains the tumor) will not cause infertility. It may actually help restore normal sperm production if the tumor is confined only to the testicle itself. After the diagnosis of testicular cancer with radical orchiectomy, we encourage our patients to perform sperm banking prior to any additional therapy to help cure the disease even if they are not planning to have any more children in the future. Chemotherapy and radiation can lead to temporary infertility for 1-2 years, but in a smaller percentage of patients, the infertility can be permanent.
Testicular Cancer Infertility Surgery
Surgery (RPLND) does not cause infertility with regards to sperm production, but can affect ejaculation when the nerves are involved by disease or affected during surgery. This can also lead to difficulty with conceiving. At Comprehensive Urology, our physicians specialize in a newer nerve-sparing RPLND to help preserve ejaculatory function. Ask your doctor if you are a candidate for this type of procedure.
Seminoma
 After determining the type of testicular cancer and the stage of the disease, our physicians will determine the most effective treatment options to offer the highest likelihood for cure and preservation of quality of life. The type of therapy for each patient will depend on the type of cancer they have and the extent of progression of the tumor. In certain situations, patients with testicular cancer will require multimodal therapies (a combination of surgery and chemotherapy or radiation therapy). Our surgeons team with highly experienced hematologists-oncologists and radiation therapists and will create and lead the multidisciplinary team to provide the most optimal therapies for our patients who require this approach.
After determining the type of testicular cancer and the stage of the disease, our physicians will determine the most effective treatment options to offer the highest likelihood for cure and preservation of quality of life. The type of therapy for each patient will depend on the type of cancer they have and the extent of progression of the tumor. In certain situations, patients with testicular cancer will require multimodal therapies (a combination of surgery and chemotherapy or radiation therapy). Our surgeons team with highly experienced hematologists-oncologists and radiation therapists and will create and lead the multidisciplinary team to provide the most optimal therapies for our patients who require this approach.
Treatment options for testicular cancer include:
- Surgery – Retroperitoneal Lymph Node Dissection (RPLND)
- Chemotherapy
- Radiation Therapy
Chemotherapy
Chemotherapy may be an option for treatment of early stage disease considered possibly spread to the abdomen, or more advanced disease as well. It may be considered in some cases as part of the treatment plan in conjunction with surgery. The side effects depend on the type of chemotherapy used, and can include cardiovascular side effects, fatigue, and infertility. Our team will closely work with you to help determine if this is a good option to help treat your disease, and will work closely with the medical oncology doctors to follow the cancer while the disease is being treated.
Radiation Therapy
Radiation treatment is predominantly used for the pure seminoma type of testicular cancer. This type of treatment includes high energy radiation beams targeted to the groin where the seminoma has the highest risk of spread. It is a highly effective and potentially curative treatment, with the potential risks including fatigue, skin irritation and infertility, which is usually temporary.
Many men experience decreased sperm counts with testicular cancer itself, which often improves after treatment. Some of the cancer treatments above can also cause infertility as well.
Nonseminoma
 If you suspect you have testicular cancer or have been recently diagnosed, it is important to understand that this disease is one of the most treatable types of cancer. As with most cancers, the treatment options will depend on the type and stage of the disease. For example, if the cancer develops within the cells that will become sperm cells, it is called seminoma, which typically requires a certain set of treatments, whereas cancer that develops within other types of cells in the testicle, it is called nonseminoma, which requires a slightly different set of treatments.
If you suspect you have testicular cancer or have been recently diagnosed, it is important to understand that this disease is one of the most treatable types of cancer. As with most cancers, the treatment options will depend on the type and stage of the disease. For example, if the cancer develops within the cells that will become sperm cells, it is called seminoma, which typically requires a certain set of treatments, whereas cancer that develops within other types of cells in the testicle, it is called nonseminoma, which requires a slightly different set of treatments.
In order to receive an accurate diagnosis and personalized treatment plan for nonseminoma, please do not hesitate to get in touch with the experienced and dedicated team at Comprehensive Urology in Los Angeles. Our urologists are highly trained and have access to the most advanced treatment options and technologies at Cedars-Sinai Medical Hospital. Call (310) 499-2756 or contact us online today!
Diagnosing Nonseminoma
The most common signs and symptoms associated with testicular cancer, whether it is seminoma or nonseminoma, include pain in the testicle, a sensation of heaviness in the scrotum, swelling of a testicle, a lump or mass in on or both testicles, back or lower abdomen pain, and even pain or lumps in other parts of the body.
The exceptional urologists at Comprehensive Urology will conduct the following tests to identify testicular cancer:
- Physical examination
- Abdominal and pelvic CT scan
- Chest x-ray
- Blood tests
- Ultrasound of the scrotum
- Removal of one or both testicles
Once the type and stage of the cancer is accurately identified, your urologist will create a customized treatment plan to eliminate the cancer.
Treatment Options for Nonseminoma
Nonseminoma occurs as four different types: embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma. Depending on the type and stage (severity) of the nonseminoma, the following treatments may be necessary:
- Surgery (Orchiectomy) – Removal of part or all of one or both testicles.
- Active Surveillance – The earliest stages of testicular cancer may not require immediate treatment beyond surgery. Instead, a urologist will schedule regular appointments to monitor recurrence of the disease in order to avoid unnecessary or excessive treatment.
- Radiation – Any remaining cancer cells left after surgery are destroyed with high-energy radiation beams. Radiation typically targets the lymph nodes throughout the body in which cancer cells may have spread.
- Chemotherapy – Intravenous drugs are administered to kill remaining cancer cells left behind after surgery.
If you or someone you love has been diagnosed with testicular cancer, it is crucial to work with a team of testicular cancer doctors who not only have extensive experience, but also a strong track record for achieving the best possible outcome for their patients, such as Comprehensive Urology. While testicular cancer is treatable, a dedicated team will help monitor and treat recurrence or complications that may occur later on.
Retroperitoneal Lymph Node Dissection (RPLND)
One of the most common tactics for diagnosing whether the testicular cancer has metastasized or preventing the disease from spreading to other parts of the body is to remove the lymph nodes in the retroperitoneum. The lymph nodes are located throughout the entire body, and when testicular cancer spreads beyond the testis, the main route is typically through the lymphatic system, starting with the lymph nodes in the back of the abdomen. RPLND is a diagnostic or preventative measure that is very often used as a precursor or alternative to chemotherapy.
Not every patient who has been diagnosed with testicular cancer will need to have the retroperitoneal lymph nodes removed, so it is very important to discuss your treatment options with the board-certified urologists at Comprehensive Urology to determine the best treatment plan possible.
What to Expect During RPLND
RPLND is performed under general anesthesia and can take up to six hours depending on the stage and type of cancer. The surgeon will make an incision from the sternum to a few inches below the navel in order to locate and remove the appropriate lymph nodes. In some cases, the procedure may be performed with laparoscopic instruments or a robotic surgical system to reduce the number of incisions, however, traditional RPLND is currently the most reliable and effective form of this procedure. When a patient undergoes laparoscopic or robotic surgery, chemotherapy is typically recommended to ensure that all cancer cells have been eradicated.
At Comprehensive Urology, our surgeons strongly believe in performing RPLND with an emphasis on nerve-sparing techniques in order to preserve as much normal nerve function as possible. In some cases, patients may suffer nerve damage that interferes with the nerves that control ejaculation. The team at Comprehensive Urology place great importance on protecting each client’s quality of life while also providing the most advanced medical care possible to treat testicular cancer.
Recovering from Retroperitoneal Lymph Node Dissection
The recovery period following RPLND will depend largely on the type of procedure and the extent of the dissection, as well as the patient’s overall health. Removal of the retroperitoneal lymph nodes is considered a major operation regardless of the technique used, so patients should expect to spend at least a few days in an intensive care unit, followed by a week to ten days at Cedars Sinai Medical Center before returning home. Immediately following RPLND, patients may experience one or more of the following:
- Pain around the incision site
- Nausea
- Fatigue
- Poor appetite
- Use of urinary catheter
- Constipation
- Gas cramps
Patients will be encouraged to move and walk four to six times a day to help prevent complications, such as blood clots or chest infections. The expert nursing staff will assist with breathing and leg exercises, as well as pain management until the patient is ready to return home. It may take several months before patients feel fully recovered from the operation. Patients will have a scheduled follow up visit within four to six weeks after the surgery to discuss the results and whether additional treatment is necessary. Regular check ups will be necessary to monitor for recurrence of the disease.
Potential Risks and Complications
As with any surgical operation, there are potential risks and complications associated with the removal of retroperitoneal lymph nodes. It is safe for patients to have these lymph nodes removed, however, the surgical procedure itself has a minimal risk of the following:
- Wound infection
- Bowel obstruction
- Necessary retreatment
- Nerve damage
- Retrograde ejaculation
The urologists at Comprehensive Urology strive to help patients achieve the best possible outcome and work to ensure that each patient receives the comprehensive and personalized care they need to overcome testicular cancer.
Chemotherapy

If you have been diagnosed with testicular cancer, whether Stage 1, 2, or 3, it is likely that you will need to undergo chemotherapy to ensure that the disease is fully eradicated. In many cases, chemotherapy is combined with other treatments for testicular cancer, such as lymph node removal or removal of the cancerous testicle. Every patient is unique and the board-certified urologists at Comprehensive Urology strongly believe in working closely with each patient to develop a personalized treatment plan that is suited to his needs and goals.
Testicular cancer is highly treatable, even if it has metastasized, and chemotherapy is proven effective at allowing men to safely overcome the deadly disease while maintaining quality of life and physical function in most cases.
What is Chemotherapy?
Chemotherapy is essentially the use of prescription drugs to treat a disease, such as cancer, by treating the entire body. Surgery and radiation are effective at targeting the main source of the cancer, however, chemotherapy can help kill cancer cells that may have spread to other parts of the body. The most common prescription drugs for testicular cancer chemo include a combination of cisplatin, bleomycin, and etoposide. In many cases, chemo can fully eliminate all cancer cells, preventing the disease from returning, however, some patients may use the treatment to help manage the disease by shrinking and stopping the tumor from continuing to grow.
Chemotherapy is commonly administered via oral medication or intravenously at regular intervals in order to allow the patient to rest and healthy cells to regenerate after dosages. The amount of dosages and cycles of chemo will depend on the specific drugs being used, the type of cancer, the stage of the disease, and the patient’s age and overall health. The treatments can be adjusted based on how the patient reacts and how effective the drugs are at killing the cancer cells, however, it is ideal for patients to go through the full cycles and dosages as prescribed to ensure the best possible outcome.
What are the Side Effects of Chemotherapy?
While highly effective in most cases, the anti-cancer drugs used in chemotherapy are strong and cause a variety of side effects as even healthy cells are damaged. The side effects will depend on the specific medications that are used, as well as the patient’s unique reaction. The most common side effects that testicular cancer patients experience with chemotherapy include:
- Hair loss
- Loss of appetite
- Nausea
- Vomiting
- Fatigue
- Reduced resistance to infections
- Mouth sores
- Easy bruising
- Changes in taste
- Skin discoloration, sores, or dryness
- Partial hearing loss
- Lung, kidney, or liver damage
The side effects of chemo can be unpleasant, to say the least, but they are typically only temporary. Throughout treatment, our patients have access to the best team of nurses, nutritionists, and oncologists, in addition to our expert urology team to help minimize the effects of chemotherapy as much as possible. It is important to keep track of the side effects and discuss any additional treatment options to help relieve the symptoms.
Infertility and Chemo Affects on Sperm
Patients who have had one testicle removed during their testicular cancer treatment can often maintain their fertility with the remaining testicle. However, regardless of whether a patient is planning on having children in the future, we recommend that our patients perform sperm banking prior to undergoing chemotherapy to at least keep the option of conceiving a child later on. Chemo is known to decrease the number of sperm cells and impair their ability to move, resulting in temporary infertility for a year or two. In rare cases, some patients may suffer permanent infertility.
During chemo treatments, patients are advised to use a condom when having sexual intercourse within 48 hours of the last dosage as the drugs may be present in the sperm. It is not uncommon for some cancer patients to experience a decline in sexual desire during treatment due to the physical and emotional stresses of fighting the disease. Some patients or their partners may feel anxious or fearful about physical intimacy during chemo out of concern that it may harm the cancer patient. It is important to discuss your concerns with your urologist or a counselor to help you find the answers and reassurance you need.
Follow Up and Recovering from Chemo
Fortunately, most patients do not encounter long-term side effects or consequences of chemotherapy, therefore, the recovery process is fairly quick. The time it takes to return to everyday life will depend on the patient’s overall health and the type of chemotherapy that was taken. Most patients begin to feel better in a matter of days once treatment has ended.
Once diagnosed and treated for a testicular tumor, patients will be expected to undergo follow up appointments for at least the next five years to ensure that the disease has not come back. The follow ups will typically include blood tests, CT scans, and x-rays. The frequency of follow up tests will depend on the type and stage of cancer, but it is important for patients to keep all appointments to catch any signs of new or recurring symptoms as soon as possible. If the cancer comes back, it usually occurs during the first two years following treatment, however, there are rare instances in which it may recur or another cancer develops within five years.
Radiation
 If you or someone you love has been diagnosed with testicular cancer, it is in your best interest to work with a skilled medical team to ensure the best possible outcome. Through the expert care of the urologists at Comprehensive Urology, our testicular cancer patients have had great success overcoming the disease. It is important to remember that testicular cancer is often highly treatable and the dedicated team at Comprehensive Urology in Beverly Hills have the experience and training to create a personalized treatment plan, which may include radiation, for each patient’s circumstances and needs.
If you or someone you love has been diagnosed with testicular cancer, it is in your best interest to work with a skilled medical team to ensure the best possible outcome. Through the expert care of the urologists at Comprehensive Urology, our testicular cancer patients have had great success overcoming the disease. It is important to remember that testicular cancer is often highly treatable and the dedicated team at Comprehensive Urology in Beverly Hills have the experience and training to create a personalized treatment plan, which may include radiation, for each patient’s circumstances and needs.
Is Radiation Necessary?
When treating testicular cancer, the ideal treatment options will depend on the specific type and stage of the disease. Seminomas, for example, after often treated with surgery and radiation. In some cases, the cancerous tumors are removed with the entire testicle in a procedure called an orchiectomy. Once removed, radiation therapy may be recommended to eliminate any possible remaining cancer cells in order to completely clear the body and prevent recurrence.
Radiation is a highly effective method for killing cancer cells, especially if they have spread to other parts of the body, such as the lymph nodes.
What to Expect During Radiation Therapy
Radiation therapy can be administered externally or internally. External radiation therapy uses high-energy beams, often X-rays, which are directed at certain parts of the body to kill cancer cells. The patient lays on a table while the external beam radiation machine aims the energy beams at the testicles and other areas that may have cancer cells. Internal radiation therapy involves a radioactive substance that is placed directly in or near the cancer in a “seed,” needle, wire, or catheter in order to kill the cancer cells.
Following radiation therapy, you may experience the following:
- Fatigue
- Nausea
- Diarrhea
- Redness
- Irritation of the skin around the groin and other treated areas
The possible side effects typically improve over time after treatment.
Infertility Issues
Radiation often causes infertility when treating testicular cancer, so it is important to discuss options for preserving your sperm before treatment. Comprehensive Urology encourages our patients to undergo sperm banking before surgery or radiation to preserve their reproduction options, whether they want to have children or not. In some cases, radiation may only cause temporary infertility for one to two years, but we encourage our patients to keep their options open.
Contact Comprehensive Urology Today
If you’re at risk of testicular cancer and wish to seek testicular cancer treatment in Beverly Hills, please contact Comprehensive Urology today. To make an appointment or to speak with a testicular cancer doctor in Los Angeles, please call (310) 499-2756.
Next, read about Incontinence.