 Although the majority of people affected by urinary incontinence are women, many men develop the condition as well. Urinary incontinence (UI) is the accidental or unintentional leakage of urine.
Although the majority of people affected by urinary incontinence are women, many men develop the condition as well. Urinary incontinence (UI) is the accidental or unintentional leakage of urine.
It is a common misconception that developing incontinence is an inevitable part of aging, but this is not exactly true. Men, however, are more likely to suffer from the condition as they age. Please do not hesitate to call (310) 499-2756 or make an appointment online today to learn more about personalized treatment options for BPH.
What Is Male Incontinence?
UI affects many people, but the problem often goes undiagnosed. It refers to the loss of bladder control and ranges from minor to severe. UI may prevent a man from performing normal activities and enjoying everyday life, and in some instances, impacts an individual emotionally, psychologically, and socially.
People who understand UI and its symptoms can identify the problem before it escalates. As a result, these individuals may be better equipped than others to treat the issue and enjoy long-term UI relief.
Types of Urinary Incontinence in Men
There are different types of urinary incontinence, or unintentional loss of urine, in men, including stress incontinence, urge incontinence, and overflow incontinence. Some men may have one or a combination of all three.
- Stress Incontinence: Refers to the uncontrollable loss of urine when pressure is exerted on the bladder. Leakage of urine may occur during actions such as coughing, sneezing, and lifting. Stress incontinence in men may occur after prostate surgery, neurologic injury to the brain or spinal cord, or trauma. Men may also become more susceptible to stress incontinence as they age.
- Urge Incontinence: Involves the involuntary loss of urine followed by and sudden unstoppable urge to urinate. Common urge incontinence triggers in men include drinking a small amount of water, hearing running water, touching water, or being in a cold setting. In some instances, anxiety, liquids, or medications cause urge incontinence. Additionally, urge incontinence has been linked to stroke, Parkinson’s disease, multiple sclerosis, and other medical conditions that can damage the brain, bladder nerves, spinal cord, or sphincter nerves.
- Overflow Incontinence: Characterized by constant dribbling of urine, accompanied by frequent, yet small urination. Overflow incontinence is commonly associated with nerve damage from diabetes or other diseases that weakens the bladder muscles. Additionally, overflow incontinence often occurs from a blockage of urine from an enlarged prostate (BPH).
- Functional Incontinence: Occurs due to a physical disability, external obstacles, or cognitive or communication issues that prevent an individual from reaching a place to urinate before accidental leakage. Examples of functional incontinence include a man who cannot walk to a restroom in a timely manner due to arthritis, or an Alzheimer’s patient who may not plan ahead for a trip to a restroom.
- Transient Incontinence: Refers to UI that lasts only a short period of time. Transient incontinence is associated with certain drugs or medications, and it also has been linked to temporary conditions. For example, excessive caffeine or alcohol consumption may cause the bladder to fill up quickly, or a urinary tract infection may irritate the bladder, resulting in a strong urge to urinate.
Causes of Bladder Leakage in Men
The common causes of urinary incontinence in men include:
- Nerve Problems: Many diseases, conditions and injuries lead to nerve damage that may result in urination problems. The most common causes of urinary incontinence from nerve damage include long-term diabetes, stroke, Parkinson’s disease, multiple sclerosis and spinal cord injury.
- Prostate Problems: Since the prostate gland surrounds the urethra just below the bladder, conditions such as benign prostatic hyperplasia (BPH) and surgical procedures that alter the male reproductive system, including radical prostatectomy and external beam radiation, may lead to temporary or permanent bladder problems.
- Birth Defects: Men who have problems with the development of the urinary tract may be more susceptible than others to UI.
- Physical Inactivity: A lack of physical activity may cause a man’s weight to increase. Meanwhile, increased weight may contribute to muscle weakness that ultimately leads to UI.
- Obesity: Additional weight puts extra pressure on the bladder, thereby causing a man to feel the urge to urinate before the bladder is full.
- Aging: As a man ages, his bladder muscles become weaker, and the bladder’s ability to store urine decreases over time.
- Chronic Coughing: Persistent coughing puts additional pressure on the bladder and pelvic floor muscles, increasing the likelihood that a man may experience UI.
How is UI in Men Diagnosed?
It is always best to seek medical advice from your physician first as many factors may contribute to a urinary incontinence diagnoses. Your healthcare provider will examine your medical history including any major illnesses or surgeries, details about your continence issue and family history of any serious conditions. The more your doctor knows about you, including your regular food and beverage intake, as well as any medications (prescription and nonprescription), the quicker you will be able to receive a proper diagnoses along with the best treatment plan.
Generally, your doctor will request information about your pattern of urination and urine leakage. He or she may ask you to keep a bladder diary for several days prior to a consultation. This diary enables you to track the following information:
- Liquids consumed daily
- Number of times you urinate daily
- How often accidental leaks occur
- How often you feel a strong urge to urinate before leaking
Your doctor may also perform a physical examination to check for prostate enlargement or nerve damage. In some cases, tests such as ultrasound evaluations, cystoscopy and urodynamics testing will be used to isolate issues that may be related to loss of bladder control.
Male Incontinence Treatment Options
There are many treatments options available for men suffering from urinary incontinence. The treatment that your doctor recommends for you will depend on the type of incontinence you have and the severity of your symptoms. Surgical is typically seen as a last resort treatment option for very serious conditions such as infection or cancer, or if the type of UI you have is caused by a bladder blockage. If you have not been diagnosed with infection or cancer, some of the non-surgical treatment options available are:
- Behavioral Strategy – Some changes in your behavior may be enough to control symptoms of UI. These include changes to your diet, lifestyle and urinary habits.
- Medication – Certain medicines that are effective in treating urinary infections and bladder muscle spasms may also help in controlling UI.
- Biofeedback: Biofeedback can be used to stimulate the muscles of the pelvis to increase their strength and result in better urinary control.
- Percutneous Tibial Nerve Stimulation – The tibial nerve next to the ankle can be precisely stimulated with the use of an acupuncture needle and a special computer that sends the right signals via this nerve to the spinal cord, which in turn gets forwarded to the nerves of the bladder. This approach is very effective for patients with urge incontinence. Many minimally invasive therapies such.
Benign Prostatic Hyperplasia (BPH) and Incontinence
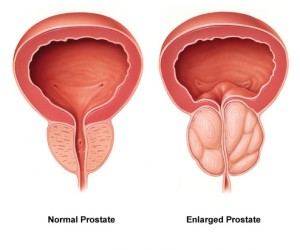 A common health condition among older men that can cause male incontinence is benign enlargement of the prostate gland or benign prostatic hyperplasia (BPH). The condition occurs when the prostate gland becomes enlarged and compresses the urethra that runs through it, interfering with urinary function. If you or someone you care about is suffering from urinary issues such as urinary urgency, leakage, or difficulty starting urination, it may be due to BPH. Fortunately, the skilled urologists at Comprehensive Urology offer a number of treatment options for men with BPH that can help relieve the symptoms and provide better control.
A common health condition among older men that can cause male incontinence is benign enlargement of the prostate gland or benign prostatic hyperplasia (BPH). The condition occurs when the prostate gland becomes enlarged and compresses the urethra that runs through it, interfering with urinary function. If you or someone you care about is suffering from urinary issues such as urinary urgency, leakage, or difficulty starting urination, it may be due to BPH. Fortunately, the skilled urologists at Comprehensive Urology offer a number of treatment options for men with BPH that can help relieve the symptoms and provide better control.
What are the Symptoms of BPH?
Benign urinary hyperplasia can cause a variety of symptoms, depending on the patient, but the most common include:
- Frequent nighttime urination (Nocturia)
- Urinary hesitancy or difficulty starting urine flow
- Slow or intermittent urine flow
- Sudden urge to urinate (Urinary urgency)
- Leakage or uncontrollable urination
- Sensation of incomplete bladder emptying
While urinary issues can be uncomfortable or embarrassing, it is important to seek medical help from a skilled urologist in order to treat the condition. If BPH is not properly addressed, patients can suffer from frequent urinary tract infections, bladder dysfunction, blockage of the kidneys, and potential kidney failure.
Treating Bladder Dysfunction Caused by BPH
Once diagnosed, BPH can be treated in order to improve bladder function and relieve discomfort. The most common treatments for BPH provided by the expert urologists at Comprehensive Urology include the following:
- Medications – There are two pharmaceutical options for treating BPH, which include Alpha Blockers and Alpha Reductase Inhibitors. Alpha blockers target and relax prostatic muscle tissue. The relaxed prostatic tissue then does not compress the urethra as much and thereby alleviates obstructive urinary symptoms. Alpha Reductase Inhibitors actually help shrink the prostate, thereby, alleviating compression of the urethra and associated obstructive urinary symptoms.
- Trans-Urethral Microwave Therapy (TUMT) – A non-surgical treatment that uses microwave energy to shrink the enlarged prostate while also widening the urinary channel. The treatment is short and maximum results are typically reached by eight or 12 weeks.
- Pelvic Floor Rehabilitation – Using physical exercise and electrostimulation of the pelvic floor muscles and nerves, patients can gain better control of their urinary function.
- Internal or External Catheter – In some cases, a catheter may be placed into the bladder to help drain urine into an external or internal pouch. This option is effective when medications do not work. It also helps patients avoid surgery while still gaining control of urinary function.
- The Urolift System – A minimally invasive surgical procedure in which tiny implants are placed within the enlarged prostate to help open up the urethra. The procedure is safe and effective, providing permanent relief with little to no downtime required.
- Trans-Urethral Resection of the Prostate (TURP) – Using an endoscopic camera, the surgeon can surgically remove portions of the prostate that block the urethra while also sealing blood vessels to improve recovery time. A catheter is used to allow the urinary channel to heal. A catheter is typically used for one day. Once the area has healed, the catheter is removed and the patient will experience significantly improved bladder function and urinary flow.
- Prostatectomy – When the prostate gland has grown so much in volume that a patient is no longer a candidate for TURP or other above mentioned treatment modalities, the enlarged and obstructive portions of the prostate can then be surgically removed. At Comprehensive Urology, such procedures (referred to as “simple prostatectomy”) are often performed robotically allowing for greater precision and excellent outcomes. In a simple prostatectomy, the entire prostate is not removed. Only the overgrown and obstructive prostatic tissue is resected, thereby optimizing urinary flow and function.
Overactive Bladder in Men
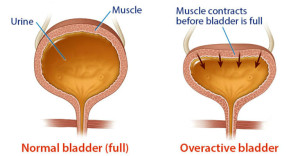 Do you find yourself suddenly feeling like you have to rush to the restroom to relieve your bladder? Have you experienced an involuntary loss of urine when you didn’t expect it? Also known as urge incontinence or spastic bladder, an overactive bladder (OAB) is essentially involuntary bladder contractions that force urine to leak out of the body. While this type of situation is often associated with women who are pregnant or recently gave birth, it can affect men as well.
Do you find yourself suddenly feeling like you have to rush to the restroom to relieve your bladder? Have you experienced an involuntary loss of urine when you didn’t expect it? Also known as urge incontinence or spastic bladder, an overactive bladder (OAB) is essentially involuntary bladder contractions that force urine to leak out of the body. While this type of situation is often associated with women who are pregnant or recently gave birth, it can affect men as well.
You do not have to live with an overactive bladder. At Comprehensive Urology, our experienced and compassionate urologists offer specialized treatments to help men successfully treat and overcome urge incontinence.
What Causes an Overactive Bladder in Men?
Temporary or long-term urge incontinence in men can occur for a wide range of reasons, including:
- Neuromuscular dysfunction as a result of spinal cord damage, stroke, diabetes, or other nervous system conditions
- Benign prostatic hypertrophy or enlarged prostate causes pressure on the bladder and surrounding nerves
- Urinary tract infections
- Medications may affect bladder function
- Advanced age
- Bladder cancer
- Previous prostatectomy, bowel resection, or other pelvic floor surgery
Whether urinary leakage occurs occasionally or on a regular basis, it is important to see your urologist to determine the cause as well as potential treatments. Urinary incontinence may be a symptom of another health issue that needs immediate attention, so do not put off a professional consultation!
Treatment Options for a Male’s Overactive Bladder
Treating an overactive bladder depends on the cause as well as the patient’s age and overall health. The urology team at Comprehensive Urology have extensive training and experience with a wide range of treatment options of male urinary incontinence and work with each patient to find the most effective treatment option for his needs. Some common options include:
- Pelvic Floor Rehabilitation – Kegel exercises and other pelvic floor muscle training can help strengthen the muscles and nerves that control the bladder.
- Timed Voiding and Double Voiding – Paying attention to fluid intake as well as the body’s schedule to accurately plan when to use the restroom, as well as emptying the bladder twice if necessary.
- Medications – Modifying medication dosages that may cause incontinence as well as taking medication that reduces the symptoms of urinary leakage.
- Botox – Botox injections can help block the nerve signals that trigger overactive bladder and reduce or eliminate the strong need to urinate.
- InterStim – An implantable device that delivers electrical pulses that help modulate neural activity around the pelvic floor.
- Surgery – Removal of an enlarged prostate gland or placement of an artificial urinary sphincter, bulbourethral sling, or sacral nerve stimulator.
Sphincteric Insufficiency
 Male incontinence, which is the inability to control urine, can happen on a temporary or long lasting basis for a number of reasons. In some cases, the sphincter muscles that control urine flow become too weak to allow the body to hold urine. Fortunately, there are several treatment options available for this condition, known as sphincteric insufficiency.
Male incontinence, which is the inability to control urine, can happen on a temporary or long lasting basis for a number of reasons. In some cases, the sphincter muscles that control urine flow become too weak to allow the body to hold urine. Fortunately, there are several treatment options available for this condition, known as sphincteric insufficiency.
If you suffer from involuntary loss of urine or weak bladder control, it is important to understand that the condition is not only treatable, but may also be a symptom of a more serious health issue. In order to identify the cause and regain control of your life, get in touch with the experienced urologists at Comprehensive Urology in Los Angeles. Call (310) 499-2756 or make an appointment online today!
What Causes Insufficient Sphincter Function in Men?
The urinary sphincter may become damaged or weakened by one or a combination of the following:
- Pelvic trauma
- Previous surgical procedures
- Prostate cancer treatments, such as radical prostatectomy or radiation
- Diabetes
- Parkinson’s disease
- Multiple Sclerosis
- Stroke
In many cases, male urinary incontinence is caused by another underlying health issue, so it is important to contact a urologist to determine the exact cause and the appropriate treatment plan. Bladder issues may be embarrassing or frustrating, but the compassionate team at Comprehensive Urology can provide the solutions you need to preserve a positive quality of life.
How is Sphincter Insufficiency Treated?
There are numerous options for managing sphincteric insufficiency, from lifestyle modification to surgical operations. At Comprehensive Urology, we believe in taking a conservative approach in order to avoid over-treatment. Many patients find success without having to resort to aggressive or invasive options.
The most common non-surgical treatments for insufficient sphincter function include:
- Lifestyle modification, including limiting fluid intake or avoiding alcohol and caffeine
- Physical therapy, such as kegel exercises to strengthen the pelvic floor muscles
- Protective undergarments, such as absorbent underwear or pads
- External penile clamps to control urine flow
Surgical treatments include:
- Catheters (exterior or interior) to collect urine
- Male sling that supports the urethra with a synthetic tape that is surgically implanted
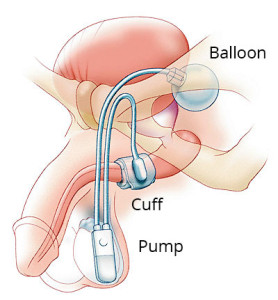
- Artificial sphincter, which controls urine flow through a pressurized balloon and cuff around the urethra that the patient can control externally
- Botox injections to decrease pressure on the bladder
- Intrinsic sphincter deficiency repair, in which collagen is inserted into the urethra to help block urine
With the trusted guidance and care of the skilled urologists at Comprehensive Urology, our patients achieve the best possible treatment for their unique needs. Our experience and access to the best medical technology allows us to not only reach an accurate diagnosis, but to also create a comprehensive treatment plan that is designed to accommodate each patient’s lifestyle and goals.
Bladder Control Medications
 Urinary incontinence, or difficulty controlling urination, is not as uncommon in men as many people think, especially in older men or men who have undergone prostate surgery. While uncomfortable or embarrassing, urinary issues such as leakage or the sudden urge to urinate can be treated with medications. If you or a family member is suffering from male incontinence, the experienced and compassionate urology team at Comprehensive Urology in Beverly Hills are highly trained at diagnosing the exact cause of incontinence as well as delivering safe, effective treatment. To learn more, please make an appointment online or call us at (310) 499-2756.
Urinary incontinence, or difficulty controlling urination, is not as uncommon in men as many people think, especially in older men or men who have undergone prostate surgery. While uncomfortable or embarrassing, urinary issues such as leakage or the sudden urge to urinate can be treated with medications. If you or a family member is suffering from male incontinence, the experienced and compassionate urology team at Comprehensive Urology in Beverly Hills are highly trained at diagnosing the exact cause of incontinence as well as delivering safe, effective treatment. To learn more, please make an appointment online or call us at (310) 499-2756.
What Medications Help Treat Male Urinary Incontinence?
It is important to understand that the best treatment for urinary incontinence in men will depend greatly on the cause and type of condition as well as the patient’s overall health. There are a number of medications that can help restore bladder control and function based on the type of condition. The most common effective medications include:
- Oxybutynin and Vesicare – Anti-spasmodic and anti-cholinergic medications, help relax the nerves that control bladder function and improve bladder capacity.
- Alpha Blockers – Such as Uroxatral, Flomax, or Hytrin, help relax prostatic muscle tissue, which may be putting pressure on the urethra, interfering with urine flow. These may be prescribed if the patient has an enlarged prostate from benign prostatic hyperplasia (BPH).
- Alpha Reductase Inhibitors – When an enlarged prostate causes urinary incontinence, alpha reductase inhibitors, such as Avodart or Proscar, can help reduce swelling of the prostate gland, relieving pressure on the urethra.
- Botox – By injecting Botox into the bladder muscles, patients can achieve up to three months of relief from incontinence. Botox injections are recommended when other medications fail.
- Myrbetriq – An oral medication, Myrbetriq reduces muscle spasms in the bladder and urinary tract, which alleviates symptoms of frequent urination, urgent urination, and urinary incontinence.
Medicine is particularly effective at treating urge incontinence, which is a type of urinary condition in which an individual suddenly experiences the urge to urinate whether or not he actually needs to.
Additional Options for Treating Male Incontinence
Finding the right treatments to help manage urinary dysfunction can take time because every patient’s condition is unique. At Comprehensive Urology, we work carefully with each client to create the best possible treatment plan to suit each client’s individual needs and goals. Medications may be highly effective when combined with other non-surgical options such as pelvic floor muscle exercises, reducing fluid intake, bladder training techniques, and acupuncture.
When urinary incontinence becomes even an occasional occurrence, do not wait to speak with a skilled urologist. Male urinary issues can be successfully treated with the expert care of the experienced urologists at Comprehensive Urology. Botox and other medications can be highly effective treatment options for many men who suffer from overactive bladders or urge incontinence. To find the best solution possible or get a second opinion, please schedule an initial consultation with our Los Angeles urologists by calling (310) 499-2756.
Peripheral Nerve Stimulation
 If you or a loved one has been struggling to overcome male urinary incontinence and conservative treatments such as lifestyle changes, medication, or physical therapy have failed, an implantable nerve stimulator may be may be just the treatment option you need. The expert urologists at Comprehensive Urology have had great success treating a range or male urinary issues with peripheral nerve stimulation. Every patient has unique needs and health goals, and our urologists are dedicated to creating personalized treatment plans to help each patient gain control and independence once again.
If you or a loved one has been struggling to overcome male urinary incontinence and conservative treatments such as lifestyle changes, medication, or physical therapy have failed, an implantable nerve stimulator may be may be just the treatment option you need. The expert urologists at Comprehensive Urology have had great success treating a range or male urinary issues with peripheral nerve stimulation. Every patient has unique needs and health goals, and our urologists are dedicated to creating personalized treatment plans to help each patient gain control and independence once again.
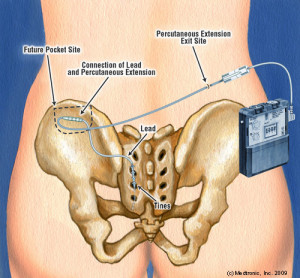
What is Peripheral Nerve Stimulation?
Peripheral nerve stimulation is essentially a small electrical device that is implanted in the patient’s body to deliver electronic pulses to specific nerves that run to the brain or spinal cord. The implanted electrode can be controlled by the patient by simply turning the device on and off with an external device to achieve the desired results. When used to treat an overactive bladder or other urinary issue, the device stimulates the peripheral nerves that control bladder function, allowing patients to reduce urinary accidents. The most effective device used for peripheral nerve stimulation is the InterStim system by Medtronic, Inc.
How is the Peripheral Nerve Stimulator Implanted?
The nerve stimulation device is typically placed during a two-stage process. The first step involves placing two small wires in a patient’s lower back in order to test whether nerve stimulation will be effective. This procedure is minimally invasive and can be performed in office using a local anesthetic. The wires stimulate the S3 peripheral nerves, which send signals to the bladder. The patient wears a small stimulator box connected to the two wires for a few days to test how well the system works. When effective, patients can experience a dramatic improvement in urinary function, such as being able to sleep through a night without having to urinate or decreasing the need to self-catheterize.
If the test is a success, the patient can then have a small pacemaker and electrode through a minimally-invasive procedure. The surgeon only needs to make a few small incisions and then guide the electrode into the correct location using a fluoroscopic x-ray.
Am I Eligible for Peripheral Nerve Stimulation?
It is important to note that nerve stimulators are not recommended for every patient suffering from male incontinence. Peripheral nerve stimulation is ideal for those suffering from certain types of incontinence, such as urgency-frequency, overactive bladder, urinary retention, and urge incontinence. However, PNS is not recommended for patients who are dealing with benign prostatic hypertrophy, cancer, or other forms of urinary obstruction.
If you or someone you care about is struggling with male urinary incontinence, do not wait to schedule a consultation with the urology specialists at Comprehensive Urology. Our physicians are dedicated to helping each patient achieve the best possible outcome for their condition.
BOTOX FOR MALE URINARY INCONTINENCE
 Incontinence occurs when the sphincter muscles of the bladder fail to hold back urine, resulting in a leaky bladder or uncontrollable urine loss. The condition can occur in men for a number of reasons, such as injury, side effects of a prostatectomy, or other health condition. Fortunately, there are several treatment options available, and one of the most recent involves the use of Botox injections.
Incontinence occurs when the sphincter muscles of the bladder fail to hold back urine, resulting in a leaky bladder or uncontrollable urine loss. The condition can occur in men for a number of reasons, such as injury, side effects of a prostatectomy, or other health condition. Fortunately, there are several treatment options available, and one of the most recent involves the use of Botox injections.
If you or a family member is suffering from male incontinence, the dedicated urology team at Comprehensive Urology in Los Angeles are skilled at diagnosing the exact cause of incontinence and then delivering effective treatment. To learn more, please contact us online or call (310) 499-2756.
Treating Male Incontinence with Botox
While commonly known as a cosmetic treatment for facial wrinkles, researchers have found that Botox (botulinum A toxin) injections can help relieve the constant urge to empty one’s bladder or urine leakage. By injecting Botox directly into the sphincter muscles of the bladder, patients gained better control of their bladders and experienced a drastic drop in the number of urinary incontinence episodes they experienced each day.
Botox works by temporarily blocking nerve signals sent to and from the brain, essentially paralyzing the muscles. When used for overactive bladders, Botox can help relieve spastic muscle active around the bladder that causes the urge to urinate or even leakage.
What to Expect During a Botox Treatment
In order to administer Botox injections into the bladder muscle, the urologists at Comprehensive Urology will first inject a local anesthetic to numb the bladder via catheter. A microscope is passed into the urethra and the bladder in order to insert a very small needle that is used to place several injections into the bladder. The procedure is fairly simple and can be performed in the doctor’s office without the need for recovery time or a hospital stay.
Patients typically begin to notice the Botox working within a week to two weeks following the procedure. While the effects are not permanent, patients may enjoy up to six or eight months of relief before returning to get another series of injections. Your urologist will monitor the effect that Botox has on your bladder muscles to determine whether an alternative treatment should be used to prevent damage to the nerves and muscles of the bladder.
It is important to note that Botox injections may not be an ideal treatment for everyone. Each patient’s condition is unique and may require a series of alternatives to reach the best solution possible.
InterStim
 If you experience difficulty controlling your bladder, resulting in involuntary leakage or a sudden urge to urinate, it may be more than an embarrassing problem. For men, an overactive bladder is often a symptom of other medical issues that require expert attention, such as nerve or muscle damage in the urinary system. When behavioral modification, medication, and other treatments for male incontinence do not work, sacral nerve stimulation with the InterStim system may be recommended.
If you experience difficulty controlling your bladder, resulting in involuntary leakage or a sudden urge to urinate, it may be more than an embarrassing problem. For men, an overactive bladder is often a symptom of other medical issues that require expert attention, such as nerve or muscle damage in the urinary system. When behavioral modification, medication, and other treatments for male incontinence do not work, sacral nerve stimulation with the InterStim system may be recommended.
At Comprehensive Urology, our expert urologists understand that every patient is unique and requires personalized care. When treating male urinary incontinence, we focus on conservative treatment methods before moving on to more involved procedures in order to find the most effective, minimally invasive treatment for each patient. Call (310) 499-2756 or contact us online today!
What is the InterStim System?
The InterStim neurostimulator system is an implantable medical device designed for sacral nerve stimulation therapy. The small device is implanted into the lower back, such above the tailbone in order to send mild electrical pulses to the sacral nerves that are connected to bladder, sphincter, and pelvic floor muscle function. The electrical pulses may provide the following effects:
- Reduce the sensation of a sudden need to urinate
- Improve nerve signal communication between the brain and the bladder
- Reduced frequency or urgency of incontinence episodes
- Reduced need for catheterization
The InterStim neurostimulator system can be placed during a simple outpatient procedure in which the urologist will numb the patient’s lower back and then insert a test electrode to ensure the neurostimulator is correctly placed and effective. The test electrode or lead will be in place for three to seven days before moving on to the actual InterStim unit. An external stimulation device will be attached to the electrode in order for the physician and patient to control when and how much to stimulate the nerves. The stimulation is often described as a vibration or pulling sensation.
Who is Eligible for an InterStim System?
Not every individual who suffers from male incontinence will be a good candidate for InterStim. The neurostimulator system is ideal for those who have tried other conservative treatments that did not work. InterStim is recommended for those suffering from an overactive bladder, urge incontinence, urinary retention problems, or urgency-frequency.
InterStim treatment is not recommended for those who suffer from stress incontinence or urinary obstructions, such as cancer, benign prostatic hypertrophy or narrowing of the urethra.
InterStim therapy has been found to be highly effective for certain individuals, however, it is important to work with an experienced urologist to find not only an accurate diagnosis, but also trusted guidance and treatment.
Male Urethral Sling
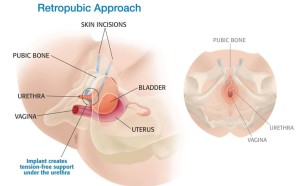 In some cases, when men suffer from urinary incontinence, it is often caused by urinary sphincter weakness following a prostatectomy or transurethral resection of the prostrate. In order to help support the urinary sphincter, it may be necessary to have a urethral sling surgically implanted. Fortunately, the male urethral sling is a fairly simple operation that requires very little recovery time.
In some cases, when men suffer from urinary incontinence, it is often caused by urinary sphincter weakness following a prostatectomy or transurethral resection of the prostrate. In order to help support the urinary sphincter, it may be necessary to have a urethral sling surgically implanted. Fortunately, the male urethral sling is a fairly simple operation that requires very little recovery time.
If you are looking for a solution to male urinary issues, please do not hesitate to contact the exceptional urology team at Comprehensive Urology in Los Angeles. Our team has extensive training and experience with diagnosing and treating a wide range of urological issues in men and can help you find the best treatment possible.
What is the Male Urethral Sling?
A urethral sling is essentially a small support system made of synthetic mesh or tissue taken from the patient’s thigh or abdomen. The sling is placed at certain points along the urethra to help reposition and strengthen the bladder system. The sling helps support the urethra and urinary sphincter, preventing unexpected urine leakage or difficulty with urine retention.
What Does the Procedure Entail?
Surgically implanting a male urethral sling is typically a minimally invasive procedure that can be performed as an outpatient procedure. The operation requires only a few small incisions in the groin between the base of the scrotum and the anus. The sling is permanently placed around the urethral bulb, where it will apply a slight pressure to the urethra. Most patients will also have a catheter for a short amount of time to help with emptying the bladder as the operation site tends to be swollen immediately after surgery. Once the swelling subsides, patients can begin urinating on their own with increasing improvement for the next few weeks.
The Benefits of a Male Urethral Sling
The male urethral sling has been found to be highly effective for many patients suffering from less severe forms of incontinence. The insertion procedure is minimally invasive, which means that it takes much less time for a patient to recover from as there are fewer incisions and less blood loss. Patients also may return home within the same day or spend a single night at the hospital. The sling does not require any manipulation to be effective and patients can return to normal activities after just a few weeks.
To learn whether you or a loved one is eligible for a male urethral sling, get in touch with the qualified team at Comprehensive Urology. A urethral sling is not suitable for every patient, however, a dedicated urologist with years of experience can help determine whether the procedure is safe and effective, depending on the unique circumstances of each patient.
If you or someone you care about suffers from male urinary incontinence, do not wait to schedule a consultation with the urology specialists at Comprehensive Urology. Our physicians are dedicated to helping each patient achieve the best possible outcome for their condition.
Artificial Urinary Sphincter
 If you suffer from significant stress incontinence and conservative treatment methods, such as medications or physical therapy, have not worked, you may need more advanced support for the structure of your bladder and urinary sphincter. At Comprehensive Urology, our exceptional urologists have extensive experience helping patients overcome mild to severe male urinary issues with a thorough treatment plan that is customized to each patient’s needs and goals. In the event that a patient is suffering from severe exertional leakage, many of our patients have found success with an artificial urinary sphincter.
If you suffer from significant stress incontinence and conservative treatment methods, such as medications or physical therapy, have not worked, you may need more advanced support for the structure of your bladder and urinary sphincter. At Comprehensive Urology, our exceptional urologists have extensive experience helping patients overcome mild to severe male urinary issues with a thorough treatment plan that is customized to each patient’s needs and goals. In the event that a patient is suffering from severe exertional leakage, many of our patients have found success with an artificial urinary sphincter.
What is a Male Artificial Urinary Sphincter?
An artificial urinary sphincter is a device that simulates the body’s urinary sphincter by applying and releasing pressure on the urethra to control urine flow. The device has three components that are implanted in the groin: a fluid filled reservoir, a urethral compression cuff, and an activation pump, which are all connected with unidirectional valves.
The fluid filled reservoir is placed near the bladder, where it acts as both a pressure regulator and a fluid reservoir for the device. The urethral compression cuff is placed around the urethra or the bladder neck where it will apply enough pressure to help the bladder retain urine until the patient is ready to urinate. The activation pump is placed in one of the scrotal sacs. The pump is operated by manually squeezing the activator, which causes the fluid in the cuff to deflate, allowing urine to flow freely from the bladder.
What to Expect When Implanting an Artificial Urinary Sphincter
The surgical procedure to implant an artificial urinary sphincter typically takes no more than two hours and requires only a single night stay in the hospital. However, it is important to note that the artificial sphincter will remain inactive for the first four to eight weeks after the operation in order to allow the body to recover. Since patients will continue to experience incontinence, external pads or catheterization may be recommended until the artificial sphincter is activated.
Once the body has properly healed, the patient will be instructed on how to operate the device, with the sphincter activated by applying forceful pressure to the control pump within the scrotal sac. It is important to operate the pump correctly in order to empty the bladder and avoid overflow or incomplete emptying, which can lead to additional health concerns. The urologists at Comprehensive Urology have extensive experience with artificial urinary sphincters and can provide careful guidance and direction to help each patient safely and effectively operate the pump.
If you or a family member is living with male urinary incontinence, do not wait to schedule a consultation with the urology specialists at Comprehensive Urology. The condition may be caused by an underlying health issue that needs immediate medical attention. Our physicians are dedicated to helping each patient achieve the best possible outcome for their condition.
TURP/Robotic Simple Prostatectomy
 If you suffer from male urinary incontinence as a result of benign prostatic hyperplasia (BPH), a potential treatment option that has helped many men regain control and independence is a procedure called transurethral resection of the prostate (TURP). The procedure essentially involves removing a portion of the prostate in order to widen the urethra, making it easier to empty the bladder. Transurethral resection of the prostate is one of the most effective treatment options for men suffering from obstructed bladder function.
If you suffer from male urinary incontinence as a result of benign prostatic hyperplasia (BPH), a potential treatment option that has helped many men regain control and independence is a procedure called transurethral resection of the prostate (TURP). The procedure essentially involves removing a portion of the prostate in order to widen the urethra, making it easier to empty the bladder. Transurethral resection of the prostate is one of the most effective treatment options for men suffering from obstructed bladder function.
To learn more about TURP and whether you are a candidate for the procedure, please do not hesitate to contact Comprehensive Urology in Los Angeles. Our skilled urologists have years of training and experience treating a wide range of male urinary issues and can provide the professional care and treatment you deserve.
What are the Benefits of TURP?
For many patients, TURP can help alleviate many of the following symptoms caused by BPH:
- Slow urination
- Frequency-urgency urination
- Difficulty starting urination
- Interrupted urination
- Urinary tract infections
- The sensation that the bladder is not empty
- Bladder stones
- Kidney or bladder damage
- Blood in urine
The urologists at Comprehensive Urology perform TURP on a fairly routine basis, and therefore, have plenty of experience performing the procedure on a variety of patients. When undergoing any surgery, whether minimally invasive or not, it is crucial to work with a urologic team that has extensive training as well as hands-on experience.
How is TURP Performed?
While under sedation, the surgeon uses an instrument called a resectoscope that is inserted through the urethra and into the prostate area. The resectoscope allows the surgeon to visually see the surgical site and make precision incisions to trim small amounts of tissue away from the prostate. The instrument is equipped with an electrical loop that cuts tissue while also sealing blood vessels. With only minimal tissue removed, the patient does not require lengthy recovery time. The majority of TURPs take only 45 minutes to complete and are performed as an outpatient procedure.
What to Expect after TURP
Following the transurethral resection of the prostate, patients can expect to have a catheter for only one day. TURP is generally very well tolerated and in most cases there is no need for pain medications. Afterward, patients can enjoy a powerful urinary stream after undergoing a TURP. After a TURP, many of a patient’s obstructive urinary symptoms may improve.
If you or a loved one has been diagnosed with benign prostatic hyperplasia, do not wait to schedule a consultation with the urology specialists at Comprehensive Urology. Our physicians work closely with each patient to achieve the best possible outcome for their specific needs and condition.
Schedule an Appointment with an Incontinence Expert
The board-certified urologists at Comprehensive Urology specialize in treating urinary incontinence in men, as well as women. If you are interested in learning more about your condition and the treatment options available, contact our Los Angeles office at (310) 499-2756.
Next, read Female Incontinence.