Do you struggle with female incontinence; the sudden, unexpected loss of bladder control? Do you find yourself rushing to the bathroom but can’t get there in time? Urinary incontinence in women often occurs as a result of pregnancy and childbirth, aging/menopause, female surgeries (e.g., hysterectomy), dramatic weight changes, or even neurological issues such as stroke or multiple sclerosis. The severity of incontinence can range from occasional leaks to full bladder volume urine loss before making it to the bathroom.
No woman should have to deal with accidental and unwanted urinary leakage. While embarrassing, it is important to understand that there is a solution to female urinary incontinence and the dedicated expert urologists at Comprehensive Urology will help you find the female incontinence treatment that works best for you.
If you suffer from occasional or chronic female urinary incontinence, do not wait to contact Comprehensive Urology in Beverly Hills today. Our experienced team can provide the custom female urinary incontinence treatment and care you deserve to regain control of your life. Call (310) 499-2756 today!
Types of Female Incontinence
According to the National Association for Continence, more than 25 million adult Americans suffer from some form of urinary incontinence and 72% of those are women with female urinary incontinence. Urinary incontinence, a common urological condition, is the involuntary leakage of urine. Unfortunately, women afflicted with female urinary incontinence tend not to travel far from home as a result of the social stigma and embarrassment associated with it. Female urinary incontinence can occur for a wide number of reasons, but typically occurs as one or combination of the following types:
- Stress Incontinence
- Urge Incontinence
- Functional Incontinence
- Overflow Incontinence
Stress Incontinence
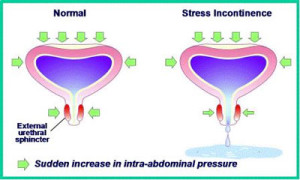
Occurs when sudden pressure is placed on the bladder by the lower stomach muscles, such as when laughing, coughing, sneezing, jumping, or jogging. The pelvic muscles may be weakened by pregnancy and childbirth or other conditions (e.g., obesity, menopause, or constipation), making urinary retention difficult. Carrying and giving birth to a child, as well as the effects of menopause, can damage the bladder and surrounding structures, leading to bladder control loss.
It is the most common kind of female urinary incontinence and affects more women than men. Approximately one in three women experience stress female urinary incontinence. The condition can have a significant impact on a female’s quality of life, as it can disrupt normal day-to-day activities.
Why Does Stress Incontinence Occur?
The layers of muscles and tissues of the pelvic floor normally support the urethra, which is the tube that carries the urine out of the body. Without these muscles and tissues, the urethra would not be kept in position. The female body goes through many changes as the result of aging and childbirth, in particular, weakening of the muscles that make up the pelvic floor. As a result, urinary retention or “holding your urine” becomes more difficult and involuntary urine leakage may occur.
Stress incontinence is known to cause urine loss during periods of exertion or when pressure is increased in the abdominal area. Leakage of urine during coughing, laughing, sneezing, or exercising is common for women with the condition.
Stress Incontinence After a Hysterectomy
Some women experience stress incontinence following a hysterectomy and should seek care from a doctor who specializes in treating incontinence. During a hysterectomy, part or all of the uterus may be removed resulting in difficulty controlling the bladder due to the muscles of the pelvic floor or sphincter being weakened. Women may experience urine leakage when putting weight or stress on the bladder from sneezing, coughing, laughing, or lifting a heavy object.
Treatment Options for Stress Incontinence
 Stress female urinary incontinence can be an embarrassing and socially traumatizing condition that can give rise to many uncomfortable situations. Fortunately, both nonsurgical and surgical treatment options are available for this type of female urinary incontinence; all have the ability to cure the condition successfully.
Stress female urinary incontinence can be an embarrassing and socially traumatizing condition that can give rise to many uncomfortable situations. Fortunately, both nonsurgical and surgical treatment options are available for this type of female urinary incontinence; all have the ability to cure the condition successfully.
Nonsurgical Treatment Options for Stress Incontinence
Pelvic Floor Exercises – Physical therapists that are specially trained in women’s health guide the patient through a series of exercises. The exercises, also known as Kegel exercises (a common combatant in female urinary incontinence treatment), are designed to strengthen the pelvic floor muscles to prevent further involuntary leakage of urine. The pelvic floor muscles are utilized whenever a woman attempts to or is successful at stopping urine flow, forming the basis and easiest explanation for Kegel exercises.
Injectable Therapy – Involves injecting medications, such as collagen, directly into the urethra. The purpose behind this method is to increase the bulk of the urethra, thus preventing involuntary leakage of urine and female urinary incontinence. The injections can be performed in a medical office with local anesthesia and are sometimes referred to as urethral bulking agents.
ThermiVa – ThermiVa can even be used to treat female urinary incontinence with no need for anesthesia and no downtime. It is a non-surgical outpatient procedure that gently heats vaginal skin tissue, resulting in shrinking and tightening. The end result is an improvement in overall skin and muscle tissue, nerve enhancement, and increased blood vessels. In appropriate patients, ThermiVa is the perfect solution for reclaiming your natural lubrication, sexual comfort, and self-confidence. Learn more about ThermiVa and other vaginal cosmetic treatments by contacting our specialists today.
Minimally Invasive Sling Surgery for Female Stress Incontinence
For some women, surgery may be a better option vs. nonsurgical female incontinence treatment. Fortunately, minimally invasive surgery for female urinary incontinence is relatively simple and can offer long-term relief from the condition without the need for an overnight hospital stay.
The most common surgical procedure performed for female incontinence treatment is called the transobturator tape (TOT) urethral sling procedure. The urologist will place a synthetic ribbon-like mesh to create a support system under the urethra. This allows the urethra to be held in place during periods of exertion or increased pressure on the abdominal area, preventing urine leakage.
Slings are usually a very popular choice for treating urinary incontinence and have high levels of success. There are two different types of slings including:
- Tension Free: Tension free slings are made from mesh and do not use any type of stitches. The body’s scar tissue holds it in place by forming in and out of the mesh, holding it in one place. Retropubic or suprapubic procedures allow the surgeon to make a small incision under the urethra and use a needle to push the sling into place. With the transobturator procedure, the surgeon makes an incision on the inside of the vagina. This lowers the risk of any type of bladder injury, and also does not use stitches to hold the mesh in place.
- Autologous: Autologous slings are made of the body’s own tissue, a donor’s tissue, or animal tissue. The sling then is placed into the abdomen and uses stitches to attach it to achieve the right amount of tension.
Since the TOT procedure is minimally invasive, patients can expect a relatively quick recovery. Most patients who undergo surgical treatment of stress female urinary incontinence are able to resume work and normal activities anywhere from 1 to 2 weeks after surgery. Although some women may need a temporary catheter for 1 to 2 days after surgery, most return to normal urination immediately.
Urge Incontinence
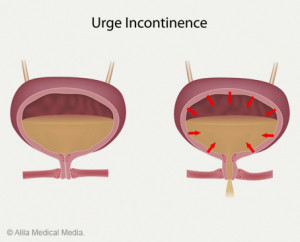
This type of incontinence occurs with the sudden urge to urinate that may be so strong that it is difficult to reach the bathroom in time before an accident occurs. Urge incontinence can occur as a result of an overactive bladder or a urinary tract infection (UTI).
Urinary incontinence affects approximately 200 million people worldwide, a large percentage of which suffer with female urinary incontinence. A common type of urinary incontinence is called urge incontinence and is characterized by a strong, sudden need to urinate. This condition is also known as overactive bladder, bladder spasms, or irritable bladder.
What Triggers Urge Incontinence?
As the bladder is filled with urine from the kidneys, it normally stretches to allow for the appropriate time for elimination. The urge to urinate does not always correspond with optimal conditions like the presence of a toilet or private appropriate place for elimination. Typically, people feel the urge to urinate when the bladder is filled with a little less than 1 cup of urine. Most people can hold more than 2 cups of urine in the bladder.
The sphincter, which is the muscle that surrounds the opening of the bladder, along with the bladder wall muscle, is responsible for helping to prevent the flow of urine. During urination, the bladder wall muscle squeezes to force urine out of the bladder. Meanwhile, the sphincter muscle relaxes to allow urine to flow from the bladder into and through the urethra. The bladder and other parts of the urinary tract, along with the nerves controlling the urinary system, must work together in order to control normal urination.
In urge female urinary incontinence, the bladder contracts when it should not. As a result, urine leaks passed the sphincter muscles. Additionally, a bladder may contract uncontrollably from problems in the nervous system or irritation in the bladder.
Although direct causes of female urinary incontinence are unclear, urge incontinence may occur as a result of:
- Bladder cancer
- Bladder inflammation
- Bladder stones
- Bladder infection
- Obstruction of the bladder opening
- Brain or nerve problems such as multiple sclerosis or stroke
- Nervous system injury such as spinal cord injury or stroke
- Enlarged prostate or BPH (benign prostatic hypertrophy) in male incontinence
When to Seek Treatment for Urge Incontinence
For some women, living with urge female urinary incontinence is merely an inconvenience that does not require a trip to a urologist. However, for others, the condition can have a negative impact on their quality of life and their ability to perform normal activities. If urge incontinence is hindering your day-to-day routines, seeking medical help from the experts at Comprehensive Urology in Beverly Hills is recommended.
These are some signs that you may need to be evaluated immediately for urge female urinary incontinence treatment:
- Pain in the pelvic region (lower stomach)
- Frequent and urgent urination (during the day and night)
- Painful, burning urination
- Ongoing symptoms for several days
Relieving Symptoms of Urge Incontinence
Fortunately, there are many nonsurgical and surgical treatment options available for this type of female urinary incontinence. Since urge incontinence is normally a chronic condition that does not have serious complications, choosing not to seek treatment will depend entirely on the person and whether or not the condition is significantly affecting their daily life. For women who are seeking relief from female urinary incontinence, here is a list of self-administered and doctor-assisted treatments:
At-Home Remedies for Urge Incontinence
Dietary Changes – Limited alcohol intake and avoidance of spicy, acidic, and sugary foods are suggested to reduce bladder irritation.
Weight Loss – Being overweight plays a factor in developing urge female urinary incontinence, so increasing physical activity will help.
Kegel Exercises – This is a preferred treatment option for urge incontinence in women (and other forms of female urinary incontinence) and is designed to strengthen the pelvic floor muscles, which control urination.
Nonsurgical Treatments for Urge Incontinence
Botox Injections – In small doses, botulinum toxin type A (Botox) can be injected into the muscle of the bladder wall in a systematic fashion. This approach causes relaxation of the bladder via the resolution of muscle spasm and can be very effective in treating patients with urge incontinence that do not respond to traditional medical therapy for female urinary incontinence. Botox for urinary incontinence is injected into the bladder and is a relatively simple and effective treatment performed in the office.
Nerve Stimulators – A small bladder pacemaker is inserted under the skin of the buttocks and hooked up to the sacral nerves, as a result light pulses are sent to the nerves of the bladder. The overactivity of the nerves to the bladder can be modulated with this approach with great effectiveness. Use of a nerve stimulator can lead to significant improvement or even complete resolution of urge female urinary incontinence.
Percutaneous Tibial Nerve Stimulation (PTNS) – PTNS is nonsurgical treatment for an overactive bladder that works by regulating the bladder and pelvic floor muscles through neuromodulation of the tibial nerve which is located in the ankle.
Female incontinence may be considered a common health issue among women, especially after giving birth, but if you suffer from leakage or the sudden loss of urine, you do not have to accept it as a part of womanhood. There are numerous female urinary incontinence therapies available depending on the many different causes of urinary incontinence in women and the dedicated urologists at Comprehensive Urology in Beverly Hills can help you find the solution you need to regain control of your life. Our team believes in working with each patient to create a customized treatment plan that works for each patient’s specific needs. To learn which female incontinence treatment option is right for you, please do not hesitate to contact us for a consultation. Call us today at (310) 499-2756 or make an appointment online.
Functional Incontinence
Means that you are able to control your bladder, however, another physical issue (e.g., arthritis, Alzheimer’s disease, or multiple sclerosis [MS]) may interfere with your ability to reach the bathroom in time.
Overflow Incontinence
Occurs when the bladder becomes overfilled because it cannot empty completely. Typically, some type of obstruction or blockage (e.g., constipation, tumor, or [in men] enlarged prostate gland) leads to the difficulty in not being able to fully empty your bladder. This condition is more common in men than women; yet, it is still a contributor to female urinary incontinence.
Mixed Incontinence
Means there is a combination of the types of urinary leakage issues listed above.
Treatments for Female Incontinence
Fortunately, there are numerous female incontinence treatment options available. At Comprehensive Urology, we understand that every patient is unique and no female urinary incontinence treatment is a one-size-fits-all solution; therefore, we provide a personalized patient-centric approach to care to help each patient find the female incontinence treatment or combination of treatments that suits her specific needs.
Treatments for female urinary incontinence include:
Behavioral Modification – Regulating fluid/food intake and bladder training (e.g., delay techniques, double voiding, and/or scheduled toilet trips) can help women suffering with female urinary incontinence regain control of their bladders and prevent overflow or other accidents.
 Medications – In many cases, medications can help relax bladder muscles and prevent the spasms that cause the sudden urge to urinate or urine leakage. Examples of medications used for female urinary incontinence treatment include anticholinergics, beta-agonists, topical estrogens (in cream, ring, or patch form), and imipramine (Tofranil, a tricyclic antidepressant).
Medications – In many cases, medications can help relax bladder muscles and prevent the spasms that cause the sudden urge to urinate or urine leakage. Examples of medications used for female urinary incontinence treatment include anticholinergics, beta-agonists, topical estrogens (in cream, ring, or patch form), and imipramine (Tofranil, a tricyclic antidepressant).
Botox – Botulinum toxin type A (Botox) injections into the muscle of the urinary bladder have been found to be effective at relaxing the nerves and muscles responsible for urge female urinary incontinence. It should be noted that Botox is generally prescribed to women only if other first-line medications have not been successful for female urinary incontinence treatment. The injections can provide several months of relief and can be repeated once the effects have worn off.
Percutaneous Tibial Nerve Stimulation (PTNS) – PTNS is a simple office procedure that requires placing a small electrode in the tibial nerve of the leg, it is possible to regulate the nerve function that triggers overactive bladder and other female urinary incontinence issues. The treatments are non-pharmacologic (non-drug), non-invasive and highly effective (up to 80% in some reports).
Interstim – Medtronic’s sacral neuromodulation system (SNS, better known as Interstim) is a procedure for female urinary incontinence treatment in which a small device (SNS) is surgically implanted in the lower back to stimulate the sacral nerves that control bladder and bowel function. The device helps women regain control of their bladder function.
Mid-Urethral Sling – During this surgical procedure, a small strip of artificial mesh or tissue is placed around the urethra (the urine channel which drains the bladder) to help support the to help support the urethra, if it becomes weak with age and often after childbirth. The procedure is often very helpful for cases of stress female urinary incontinence.
What is a Mid-Urethral Sling?
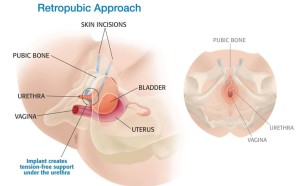 One of the most common surgical treatments for stress female urinary incontinence is a mid-urethral sling, which is essentially a method of supporting the urethra to prevent unexpected urine leakage. The sling is typically made of synthetic mesh, but, in some cases, tissue taken from the abdomen or thigh may be used. The sling may be placed at varying points along the urethra to help with urine leakage, such as directly under the bladder neck where the urethra leaves the bladder.
One of the most common surgical treatments for stress female urinary incontinence is a mid-urethral sling, which is essentially a method of supporting the urethra to prevent unexpected urine leakage. The sling is typically made of synthetic mesh, but, in some cases, tissue taken from the abdomen or thigh may be used. The sling may be placed at varying points along the urethra to help with urine leakage, such as directly under the bladder neck where the urethra leaves the bladder.
What to Expect During a Urethral Sling Procedure
A urethral sling procedure is typically minimally invasive and takes no more than 30 minutes to one hour to perform. After light anesthesia takes effect, the surgeon will make very small incisions in the vaginal area in order to place the sling around the urethra, before closing the incisions with absorbable sutures. A urethral sling procedure is highly effective and is performed as an outpatient procedure.
Many women see immediate results after the procedure, although some may need to wait a few days to a few weeks for full results. Following the urethral sling procedures, patients can typically return to normal activities within 2 to 4 weeks.
Which Medications Treat Urinary Incontinence in Women?
There are numerous medications on the market designed to treat female urinary incontinence, but it is important to discuss your options with a reliable urologist first to determine which medication is best for your condition. The type of medication will depend on the cause and type of urinary condition that you experience, as well as your overall health.
The most common medications for urge female urinary incontinence treatment are anticholinergic or antispasmodic medications, which help prevent spasms of the bladder muscles as well improve bladder capacity. These medications include tolterodine, oxybutynin, trospium, solifenacin, and mirabegron.
One of the newest medications for treating urinary incontinence in women are Botox injections. When injected into the bladder muscles, this neuromodulator relaxes the bladder muscles and reduces the spasms that cause leakage or the sudden urge to urinate. Botox can provide up to six months of relief from female urinary incontinence and is often prescribed when other medications fail.
Women who suffer from stress incontinence, which occurs when actions or activities put pressure on the bladder and cause leakage, may not be eligible for medications. In some cases, stress female urinary incontinence may be improved with physical exercises, such as Kegel exercises.
Additional Treatment Options For Female Incontinence
In many cases, medications may be prescribed for female urinary incontinence treatment in addition to a number of conservative treatment options, such as:
- Lifestyle Modification – Weight loss, scheduling fluid intake, and avoiding caffeine or alcoholic drinks can reduce incontinence issues.
- Exercise – Kegel exercises, which help strengthen the pelvic floor muscles, can provide better bladder control.
- Bladder Training – Scheduling when you go to the restroom and then gradually increasing the amount of time between restroom visits can retrain your bladder into retaining fluid for longer periods.
Every woman can successfully manage female urinary incontinence and significantly reduce the number of accidents with the careful treatment of the incontinence experts at Comprehensive Urology.
Risks and Complications of Female Incontinence Treatments
It is important to note that a urethral sling for female incontinence treatment may not be ideal for every woman. As with most surgical operations, there are possible risks and complications that may occur. It is crucial to work with a skilled urologist who has your best interests in mind and will carefully assess and explain the best female urinary incontinence treatment options for you. Potential risks following a mid-urethral sling operation include pain, inflammation, sling erosion, or difficulty urinating.
If you or someone you care about is suffering from stress incontinence or other female urinary incontinence issues, do not put off speaking with an experienced and compassionate urologist. At Comprehensive Urology, we take the time to understand each patient’s unique situation and work to find the least invasive and most effective treatment for the cause of their female urinary incontinence.
Contact A Female Incontinence Specialist
When female urinary incontinence becomes even an occasional accident, do not wait to schedule an appointment with a skilled urologist. Female urinary incontinence issues can be successfully treated with the expert care of the experienced urologists at Comprehensive Urology. To find the best female incontinence treatment solution for your specific needs or to get a second opinion, please schedule an initial consultation with our Los Angeles urologists by calling (310) 499-2756.
Next, read about Male Incontinence.