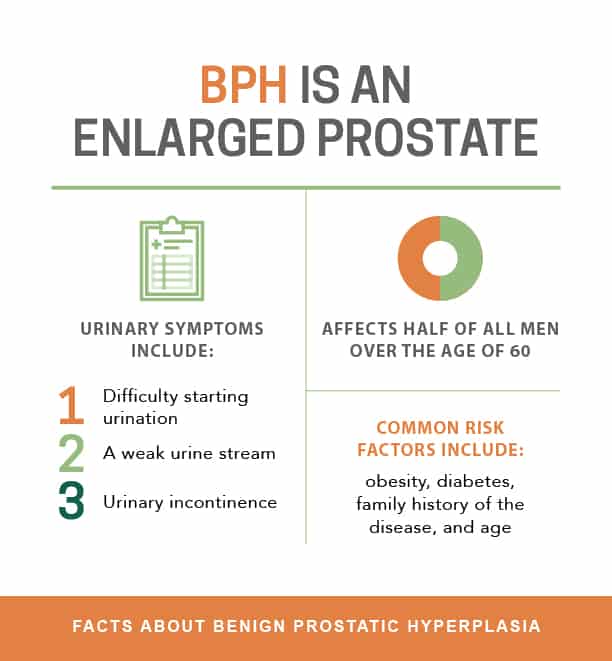
Benign prostatic hyperplasia (BPH) is another term for benign enlargement of the prostate gland. It is very common in older males, affecting approximately half of men in their 50’s and the majority of men in their 70’s and 80’s. Because the prostate gland surrounds the urethra like a doughnut, enlargement of the gland can cause urethral compression, leading to difficulty with urination.
At Comprehensive Urology, we offer a variety of treatments to help men with BPH, tailored to their specific situation. With a collective urological experience of over 125 years and over 3,000 prostate surgeries performed to date, Comprehensive Urology is Los Angeles’ top prostate treatment experts. Contact us today to schedule a consultation with our expert urologists.
BPH Symptoms
Symptoms of benign prostatic hyperplasia vary from person to person, and can include one or many of the following:
- Difficulty starting urination (urinary hesitancy)
- Slow urinary flow and having to “push” to urinate
- Intermittent flow of urine
- Sense of incomplete bladder emptying
- Having to use the restroom too often and shortly again after urination
- Having to wake up from sleep to urinate (nighttime urinary frequency interrupting sleep)
- Urinary urgency and difficulty postponing urination
- Urinary incontinence (leakage of urine)
When left untreated, BPH can lead to bladder dysfunction and physical damage to the bladder, recurrent urinary tract infections, and even obstruction of the kidneys and subsequent kidney failure.
Diagnosic Tests
 A proper diagnosis is essential to developing the optimal treatment plan for each patient with BPH. Our physicians first begin with a thorough history, including your IPSS (or International Prostate Symptom Score). BPH can result in a multitude of symptoms, and therefore it is essential that a treatment plan is based upon how BPH is specifically affecting your life. Also, many symptoms of BPH can overlap with other disorders, such as overactive bladder syndrome or urinary tract infections. Therefore, it is important to thoroughly assess each patient to make the correct diagnosis.
A proper diagnosis is essential to developing the optimal treatment plan for each patient with BPH. Our physicians first begin with a thorough history, including your IPSS (or International Prostate Symptom Score). BPH can result in a multitude of symptoms, and therefore it is essential that a treatment plan is based upon how BPH is specifically affecting your life. Also, many symptoms of BPH can overlap with other disorders, such as overactive bladder syndrome or urinary tract infections. Therefore, it is important to thoroughly assess each patient to make the correct diagnosis.
The tests used to diagnose BPH at Comprehensive Urology include the following:
- Physical Examination – A thorough physical examination is paramount for the diagnosis of BPH. Specifically, a digital rectal examination is performed by inserting a gloved finger into the rectum. This helps to determine if the prostate gland is enlarged, helps the urologist to estimate the size, and other factors, such as pain or tenderness, which may be due to infection. Rectal exams are also used to help screen for prostate cancer.
- Urinalysis – A quick dip strip test of the urine can help detect abnormalities, such as the presence of blood cells, inflammation, or infection.
- Urine Flow Test – A urine flow test measures the flow rate and amount of urine passed by the patient during a normal void. It is often used to monitor the response over time with treatment as well.
- Post-Void Residual (PVR) – Usually done with a simple bladder scan with a probe placed over the lower abdomen, a post-void residual test detects how much urine is actually left in the bladder after the patient has finished voiding.
- Ultrasound – Ultrasound of the pelvis can aid with measurement of prostate gland size/anatomy and changes in the bladder due to the enlarged prostate (such as bladder stones or deformities). It can also help detect anatomic variations in the prostate gland or even prostate tumors. Ultrasound of the kidneys can also help determine the effects of BPH on the kidneys.
- Cystoscopy – Direct visualization of the urethra and bladder by inserting a thin scope with a camera attached (called a cystoscope) after “numbing” the urethra with anesthetic gel. This invaluable test can help visualize the internal urethra and bladder with great detail and minimal to no discomfort. It is used in many instances, including in the determination of cause/degree of obstruction, the source of blood in the urine, checking for stones or tumors, removing objects from the bladder, and more.
- Urodynamic Studies – Urodynamic studies characterize sensations and pressures within the lower urinary tract, ultimately helping to characterize the bladder’s response to filling and ability to empty with normal contractions, over-activity, reduced activity, and many other voiding issues. This diagnostic test is often combined with a cystoscopy to thoroughly evaluate function and anatomy and to plan for surgery or other treatments.
Our team at Comprehensive Urology will help determine which of these evaluations may assist in the diagnosis of BPH. They may also be used to help monitor progress once treatment has been initiated.
Non-Surgical BPH Treatments
 At Comprehensive Urology, there are a multitude of treatments available for BPH. The specific treatment options are tailored to each patient’s unique situation and needs in order to provide the best possible outcome. The urological specialists at Comprehensive Urology will discuss which treatment option is best for your particular situation.
At Comprehensive Urology, there are a multitude of treatments available for BPH. The specific treatment options are tailored to each patient’s unique situation and needs in order to provide the best possible outcome. The urological specialists at Comprehensive Urology will discuss which treatment option is best for your particular situation.
- Lifestyle Modifications – For mild urinary bother due to BPH, different lifestyle adjustments will be suggested. These can include things such as reduced fluid intake before bedtime, decreased use of bladder irritants (e.g. coffee, tea, etc.), and voiding before going to bed.
- Alpha Blockers – Alpha blockers are medications that target the smooth muscle fibers inside the prostate gland and bladder, causing them to relax. This results in an improved urinary stream and increased flow, usually within days. The low side effects profile and once-a-day regimen make alpha blockers the first line of treatment for many patients.
- 5 Alpha Reductase Inhibitors – These medications block the production of potent hormones that stimulate prostate growth. They take longer to show benefits compared to the previous group of medications but, in many cases, can actually cause the enlarged prostate to “shrink” with long-term use. They can be very effective either alone or in combination with alpha blockers.
- Erectile Dysfunction Medications – Daily low-dose use of erectile dysfunction medications, such as Viagra or Cialis, has been found to improve urination in some BPH patients.
Surgical BPH Treatments
If non-surgical treatments options aren’t working, the BPH specialists at Comprehensive Urology may choose a surgical treatment method instead. Though the level of invasiveness can vary depending on the treatment, the concept of all treatments is the same: to create a larger urinary channel through the prostate gland in order to allow easier urinary flow.
REZUM® for Treating BPH
 Rezum® is the latest and most advanced transurethral procedure designed to treat benign prostatic hyperplasia (BPH) without interfering with a patient’s sexual function including erection and ejaculation. Rezum® received FDA approval for BPH treatment in 2015 after successfully passing multi-center clinical trials that proved it to be safe, minimally invasive, and possible to perform as an outpatient procedure. Patients can return to the comfort of home on the same day as the treatment. This life-changing procedure has been used with great success since 2013 and offers one of the most efficient methods for reducing or eliminating the symptoms of BPH.
Rezum® is the latest and most advanced transurethral procedure designed to treat benign prostatic hyperplasia (BPH) without interfering with a patient’s sexual function including erection and ejaculation. Rezum® received FDA approval for BPH treatment in 2015 after successfully passing multi-center clinical trials that proved it to be safe, minimally invasive, and possible to perform as an outpatient procedure. Patients can return to the comfort of home on the same day as the treatment. This life-changing procedure has been used with great success since 2013 and offers one of the most efficient methods for reducing or eliminating the symptoms of BPH.
Unlike traditional BPH treatments which involve removing all or portions of the enlarged prostate with surgical incisions, Rezum® utilizes convective WAVE® technology to gently and immediately damage only the targeted prostate tissues by causing cell death. This, in turn, allows the body to absorb the dead cells through the natural healing process later, thus de-bulking the enlarged gland. The Rezum® procedure is quick, minimally invasive (no incisions needed), and often only requires a local anesthetic. And best of all, it is so effective that patients typically do not have to undergo any additional treatments.
REZUM 3D Animation with Patient Audio from REZUM
In a nutshell, the REZUM system is a revolutionary BPH treatment for the following reasons:
- State of the Art: The newest treatment option for urinary issues due to enlarged prostate.
- Minimally Invasive: No cuts or incisions and the procedure can be done without anesthesia.
- Quick: Only one treatment session is necessary (less than 1 hour).
- Effective: “Rapid and durable improvements” noted in multi-center clinical trial.
- Safe: No sexual side effects (erections and ejaculation are not affected).
How Does the REZUM Procedure Work?
The REZUM system has a generator and a handheld device that uses water vapor (steam) which is injected through openings of a very fine needle. During the procedure, the device transforms a small amount of water into sterile steam in a controlled fashion. This steam is then transferred to the targeted prostate tissue through the retractable needle. The urologist uses direct vision (live video) to navigate the urethra and then deploys the very thin needle through the specific enlarged portions of the prostate, ensuring that healthy tissue is unaffected and only the obstructing areas are targeted.
Once the steam is injected into specific parts of the enlarged prostate gland, it transforms back into a liquid and the high temperature effectively kills the targeted prostate cells in as little as nine seconds. REZUM essentially uses convective energy to affect specific tissues without interfering with the surrounding nerves and muscle tissue that are essential to proper genitourinary function. The dead cells are eventually simply absorbed and eliminated by the body and the prostate gland as a whole is reduced in size. Within 2-3 weeks of the REZUM therapy, patients can expect to have significantly improved urination. Maximal improvement will be experienced by the three month mark.
What are the Benefits of REZUM BPH Treatment?
Following REZUM treatment for BPH, patients can expect to experience the following benefits as early as two weeks:
- Improved urinary stream
- Ability to completely empty the bladder
- No straining to urinate
- Less frequent urination
- Pain-free urination
- Less nighttime urination
Transurethral water vapor therapy is highly effective at shrinking the prostate gland and relieving urinary obstruction caused by an enlarged prostate (BPH). Unlike other BPH treatments, Rezum® does not harm the nerves and muscle tissue responsible for normal sexual and urinary function. It also does not cause the uncomfortable side effects, such as dizziness or sexual dysfunction that are seen with most BPH medications. The water vapor therapy option is ideal for patients who do not qualify for surgery due to health issues, do not wish to take lifelong BPH medications, or simply are unwilling to undergo more invasive BPH treatments and wish for a minimally invasive yet highly effective approach.
What to Expect After REZUM
After Rezum® therapy, the prostate will likely be swollen for a few days, so it is recommended that patients wear a catheter temporarily until the swelling has subsided in order to prevent urinary blockage. Unlike other methods of reducing or managing the symptoms of benign prostatic hyperplasia, patients can return to everyday activities within a few days after the procedure and do not have to adjust to uncomfortable or embarrassing side effects, such as loss of sexual ability, urine leakage, etc.
Rezum® is more than just a quick and easy procedure; it can significantly improve a patient’s quality of life while also preserving his sexual function. When nearly 75 percent of all men in the United States over the age 65 suffer from BPH and compromised sexual and urinary function as a result, Rezum® offers the best possible outcome with minimal invasiveness and without the painful or debilitating side effects.
Rezum® is not an invasive surgical procedure and, as a result, does not have a lengthy recovery process. This cutting edge treatment has a significantly lower risk of infection or other complications. Rezum® is a quick and convenient procedure that can be performed at the Comprehensive Urology office and is usually completed in less than 10 minutes. Additionally, it is covered by most insurance companies.
TURP
 TURP (transurethral resection of the prostate) is considered the gold standard surgical treatment for BPH because of its durability and efficacy as a procedure. By using an endoscopic camera and an electrical loop, our surgeons can shave away the prostatic tissue and seal opened blood vessels until a larger urinary channel is created. No incision is made on the skin and you will be under anesthesia. A urinary catheter is left to drain the bladder until the channel is healed (usually 24 to 72 hours). In most cases, the improvement in urinary flow and symptoms is dramatic.
TURP (transurethral resection of the prostate) is considered the gold standard surgical treatment for BPH because of its durability and efficacy as a procedure. By using an endoscopic camera and an electrical loop, our surgeons can shave away the prostatic tissue and seal opened blood vessels until a larger urinary channel is created. No incision is made on the skin and you will be under anesthesia. A urinary catheter is left to drain the bladder until the channel is healed (usually 24 to 72 hours). In most cases, the improvement in urinary flow and symptoms is dramatic.
A newer surgical option, called transurethral plasma vaporization and resection of the prostate (TURiP), allows our surgeons to perform a procedure almost identical to the TURP, but with several advantages. It allows vaporization of the prostate tissue as well as resection with bipolar electrical current. This current allows treatment to be performed in the setting of saline, a fluid found normally in our bodies. This, in turn, allows less risk of developing mineral abnormalities in the blood during the procedure, a problem found (although rarely) with TURP. This makes TURiP an even safer and more precise treatment of the prostate gland than the traditional TURP procedure.
For men who experienced moderate to severe symptoms of benign prostatic hyperplasia, TURP has been proven to successfully improve undesirable symptoms associated with BPH. It is still the gold standard procedure for BPH and, according to recent studies, men who underwent TURP experienced less symptoms compared with those who waited for the condition to fade away on its own.
Side Effects of TURP
Although TURP aims to improve the symptoms of benign prostatic hyperplasia, some people have experienced unwanted post-surgery side effects. The most common side effects of transurethral resection of the prostate may include:
- Bleeding After the Procedure – The bleeding gradually decreases over time and should stop completely after four weeks (but usually stops much sooner).
- Retrograde Ejaculation – Although most men are able to have erections and orgasms after TURP, some may not be able to ejaculate because the bladder neck is removed along with prostatic issue. This causes the ejaculate to enter the bladder, which will be passed out in the next flow of urine. This is completely harmless to the patient and may only disrupt fertility, but it has no effect on erections.
Less common side effects of TURP, which are rare, may include:
- Erectile Dysfunction – The inability to achieve or maintain an erection during sexual intercourse (rare, but may happen).
- Urethral Strictures – Scarring in the urinary tract that may cause even more obstruction to the urine flow.
- Urinary Incontinence – Surgery may result in the inability to hold or control the flow or urine (usually temporary and resolves more than 90% of the time in a week or two).
- Infertility – This is linked to retrograde ejaculation. Although harmless, it may result in making natural insemination impossible.
- No Change in Urinary Symptoms – Unfortunately, surgery is not effective for very few people and the undesirable symptoms of BPH may persist, including difficulty emptying the bladder completely and frequent urination at night. Generally, the latter takes a while to improve after TURP.
PVP Laser BPH Treatments
 Another newer minimally invasive surgical option is laser photovaporization of the prostate (PVP). The procedure is performed by using an endoscopic camera through the urethra, but instead of treating the tissue with an electric knife, the tissue is vaporized by utilizing a laser. The advantages of this procedure include less risk of complications (mostly bleeding) and indwelling catheter duration.
Another newer minimally invasive surgical option is laser photovaporization of the prostate (PVP). The procedure is performed by using an endoscopic camera through the urethra, but instead of treating the tissue with an electric knife, the tissue is vaporized by utilizing a laser. The advantages of this procedure include less risk of complications (mostly bleeding) and indwelling catheter duration.
Unlike traditional surgery, laser treatment is minimally invasive and can be performed on an outpatient basis under general anesthesia. The procedure involves passing a scope through the penis into the urethra and then passing a laser through the scope to reach the prostrate. The laser is used to shrink or remove excess prostate tissue that has been blocking the urethra and causing the symptoms of BPH.
Types of Prostate Laser Surgery
There are several types of prostate laser treatments available, each using the concentrated light to direct precise, intense heat at the prostate tissue. These laser treatments include:
- Holmium Laser Enucleation of the Prostate – The laser cuts through excess tissue while another instrument is used to cut these pieces down even further to be easily removed.
- Photoselective Vaporation of the Prostate – The laser melts or vaporizes the excess prostate tissue to make the urinary channel larger.
- Holmium Laser Ablation of the Prostate – This laser also melts away or vaporizes the excess prostate tissue.
The type of laser that a surgeon chooses will depend on the size of the enlarged prostate, as well as the patient’s health, and the lasers that are available. Comprehensive Urology has access to the most advanced technology and instruments available courtesy of Cedars Sinai Medical Center.
Benefits of BPH Laser Treatment
Laser therapy is one of the most commonly used treatments for an enlarged prostate because it has several advantages over traditional surgery, including:
- Reduced Risk of Bleeding – Laser therapy is minimally invasive and leaves the surrounding tissue and muscle relatively untouched. The laser can be used to precisely remove an exact amount of the prostate, therefore, patients suffer less blood loss and can heal much quicker.
- Shorter Recovery Time – Recovering from minimal incisions on the prostate is much quicker for most patients compared to traditional operations.
- Limited or No Hospital Time – Patients can often return home the same day or the next day after the treatment, whereas other procedures may require several days of hospital time.
- Less Time with a Catheter While Healing – Following many prostate surgeries, patients often need a catheter for the first few days or weeks to ensure urinary function, however, after laser surgery, patients are able to recover quickly enough that they may need a catheter for less than a day.
- Immediate Improvement in Urinary Function – Patients typically experience a noticeable improvement in urinary function right after laser therapy, unlike other procedures, which may take several weeks to see any results.
Risks of Laser Treatments for BPH
Laser treatment, especially when conducted by a skilled urologist, is less likely to cause serious or long-term side effects or complications. However, as with any operation, there are potential risks, including:
- Urinary tract infections
- Difficulty urinating
- Narrowed urethra
- Retrograde ejaculation (dry orgasm)
- Erectile dysfunction
- Need for follow-up
TUMT and Microwave Treatment for BPH
 Transurethral microwave thermotherapy (TUMT) is a non-surgical option recommended for men who have not responded well to medications or other conservative BPH treatment methods. Microwave therapy is minimally invasive and can be safely and comfortably performed on an outpatient basis. Only a single session is necessary to achieve the best possible outcome.
Transurethral microwave thermotherapy (TUMT) is a non-surgical option recommended for men who have not responded well to medications or other conservative BPH treatment methods. Microwave therapy is minimally invasive and can be safely and comfortably performed on an outpatient basis. Only a single session is necessary to achieve the best possible outcome.
TUMT uses microwave energy to heat the prostate, which causes the tissue to tighten and shrink, effectively relieving pressure on the urinary channel that runs through the prostate. The procedure is non-surgical and minimally invasive because it requires simply inserting a special urinary catheter into the urethra. A microwave antenna within the catheter is activated and emits microwaves from inside the prostate, while a cooling fluid is also circulated around the antenna to avoid causing any damage to the wall of the urethra.
In most cases, the procedure may take no more than 30 minutes to one hour and requires only a local anesthetic. It is recommended that patients have a friend or family member drive them home afterward.
Recovering from BPH Microwave Therapy
While microwave therapy leaves the surrounding tissue intact, the procedure can cause swelling and mild discomfort for a few days. Voluntary urination may be difficult during this short recovery period, which is why many patients are catheterized to assist with urination while the prostate and urinary tract heal.
In order for a patient to experience the full results of the microwave therapy, the body must absorb the prostatic tissue that has been treated, which usually occurs between six to 12 weeks. During this time, patients will not notice any changes in BPH symptoms; however, the full results are gradual but long-term.
Benefits of Microwave Therapy
BPH microwave therapy is proven to be safe and effective at relieving the uncomfortable symptoms and risks of benign prostatic hyperplasia. As a minimally invasive procedure, patients do not have to go through the physical and emotional stress of undergoing surgery, while also enjoying a marked improvement of urinary function. Unlike surgery, there is a reduced risk of damage to surrounding muscle and tissue, which means that patients can maintain their quality of life. Microwave therapy is also less likely to cause side effects than traditional surgery, which allows the surgeon to help preserve quality of life.
Additional benefits include:
- Patients can return home the same day as the procedures
- Reduced risk of bleeding
- Shorter recovery time
- No lengthy hospital stays
- Long-lasting relief of BPH symptoms for two to five years or more
- Typically covered by Medicare and other private insurance plans
Risks of Microwave Therapy
While the risks associated with microwave treatments are minimal, the procedure can cause an increased risk of urinary tract infection, particularly during the one to two week period in which the patient is catheterized. Other potential side effects include:
- Urinary retention
- Short-term incontinence
- Blood in the urine
- Difficult or painful urination
- Sexual dysfunction
- Abdominal pain
- High fever
UroLift® for BPH Treatment
The UroLift system is one of the latest a minimally-invasive procedures for treating BPH. This state-of-the-art system provides permanent relief from the symptoms of BPH without the cutting, removing part of the prostate or even heat. UroLift essentially uses tiny implants to hold the enlarged prostate tissue out of the way of the urethra, allowing the patient to return to his normal physical activities in as little as two weeks. Many patients experience only minor discomfort during the recovery period. The procedure is performed in-office with an experienced urologist and patients may return home the same day without a catheter.
Since UroLift is a minimally invasive approach to BPH, recovery time after the procedure is usually quick. Furthermore, unlike other BPH procedures, recovery normally does not require the temporary use of a catheter. Studies have shown that this procedure has been successful in preserving sexual function. It is also not known to cause serious side effects such as retrograde ejaculation or permanent erectile dysfunction.
What to Expect During the UroLift Treatment
The urologists at Comprehensive Urology are exceptionally skilled in performing UroLift. This treatment can be performed under local or general anesthesia, either in a doctor’s office or hospital.
First, the urologist will insert a delivery system through the urethra in order to determine the precise area(s) of the prostate tissue to be pulled back. The urologist will then insert a small needle into the sheath, which will be used to stitch the tissue. The number of implants (stitches) will vary depending on the size and shape of the obstructive tissue. Once complete, the instruments and delivery system are safely removed.
Like many urological conditions and their corresponding procedures, the UroLift system may have some side effects, including:
- Blood in the urine (hematuria)
- Decreased urine flow
- Incomplete emptying of the bladder
- Pain/burning during urination
- Urgent urination
Simple Prostatectomy
 Simple prostatectomy is a BPH treatment option recommended mostly for men who have a very large prostate. If signs of bladder diverticula or bladder stones are present, this procedure may also be recommended.
Simple prostatectomy is a BPH treatment option recommended mostly for men who have a very large prostate. If signs of bladder diverticula or bladder stones are present, this procedure may also be recommended.
Men who are most suitable to undergo this procedure should generally be in good health, which means if you have been treated for prostate cancer before, an open prostatectomy cannot be done.
Types of Open Prostatectomy
Simple prostatectomy involves the surgical removal of the prostate gland and is usually done under general or spinal anesthetic. Patients who undergo open prostatectomy are normally required to stay in the hospital anywhere from two to three days and will require four to six weeks of recovery time. There are three ways this procedure can be performed for BPH treatment:
- Suprapubic Prostatectomy – Involves opening the bladder in order to remove the inner portion of the prostate gland through the bladder. Upon completion, two catheters are placed in the bladder, one of which is placed through the urethra. The other is inserted through an opening made in the lower abdominal wall. The catheters are not removed until three to seven days after surgery.
- Retropubic Prostatectomy – Involves moving the bladder aside to in order to remove the inner prostate tissue without entering the bladder. After this procedure, a catheter is placed in the bladder through the urethra and cannot be removed for an entire week after surgery.
- Robotic Simple Prostatectomy – Advances in surgical technology now allow a simple prostatectomy to be done robotically using the da Vinci surgical robotic system. With a robotic approach, much smaller incisions are made and precise surgical techniques are utilized, leading to excellent outcomes and relatively minimal risk for bleeding.
Due to the complexity of the procedure, open prostatectomy is only reserved for generally healthy men who have very large prostates. Although this is an effective way to achieve relief from BPH symptoms, complications can occur, including bleeding and infection.
Frequently Asked Questions
Q: What is BPH?
Q: What is the prostate?
Q: When does BPH typically occur?
Q: Who is more prone to developing BPH?
- Are 40 years old or over
- BPH runs in the family
- Diagnosed with obesity, heart and circulatory disease, type 2 diabetes
- Lacks physical activity
- Has erectile dysfunction
Q: What are the symptoms associated with BPH?
- Frequent urination (eight or more times per day)
- Urgent urination (inability to delay urination)
- Difficulty starting a urine stream
- Dribbling at the end of urination
- Nocturia (frequent urination during sleep)
- Urinary incontinence (accidental loss of urine)
- Pain after ejaculation or during urination
- Unusual color or smell in urine
Q: What causes benign prostatic hyperplasia?
- As men age, the amount of active testosterone in their blood decreases, which leaves a higher proportion of estrogen within the prostate. Scientific studies have suggested that estrogen may promote prostate cell growth.
- Other research suggests that when there is a drop in blood testosterone levels, older men continue to produce and accumulate high levels of DHT (a male hormone that is linked to prostate development and growth). Some believe that the accumulation of DHT may encourage prostate cells to continue to grow.
Q: What are the complications that may arise with BPH?
- Acute urinary retention
- Chronic urinary retention
- Blood in the urine
- Urinary tract infections (UTIs)
- Bladder damage
- Kidney damage
- Bladder stones
Q: When can I expect to see results of my surgical treatment for BPH?
Q: : What is the average hospital stay for TURiP and PVP?
Q: How long until I can return to my normal activities?
Contact a BPH Specialist
The skilled doctors at Comprehensive Urology are leaders in BPH treatment. If you are interested in learning more about your treatment options, please contact us today.
Next, learn more about prostate cancer.